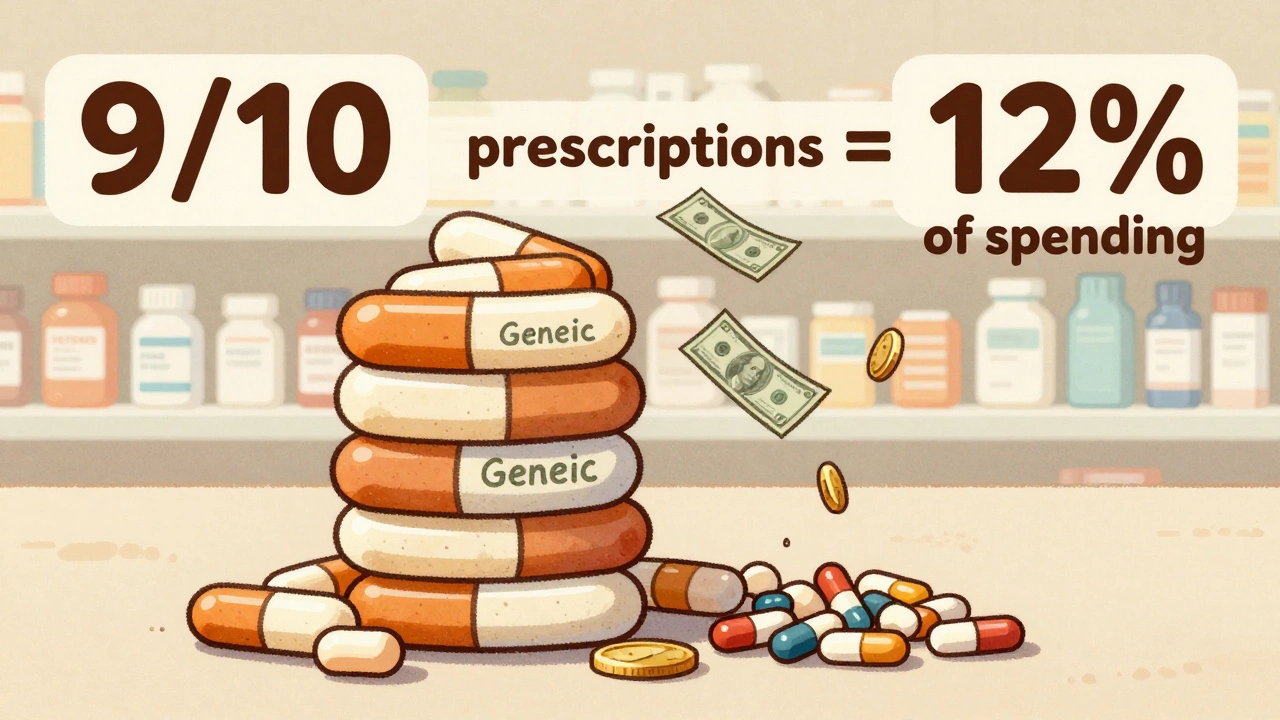
Every year, Americans fill over 3.9 billion prescriptions for generic drugs. That’s 9 out of every 10 prescriptions written. But here’s the kicker: those same generics make up just 12% of total drug spending. Meanwhile, brand-name drugs, which account for only 10% of prescriptions, soak up 88% of the money spent on prescriptions. This isn’t a glitch. It’s the math of savings.
How Much Do Generics Actually Save?
In 2023, generic and biosimilar drugs saved the U.S. healthcare system $445 billion. That’s not a guess. That’s from Serve Your Rx’s analysis of drug launches and pricing data. To put that in perspective, it’s more than the entire annual budget of the Department of Education. And it’s not just big systems saving money-individuals are feeling it too.
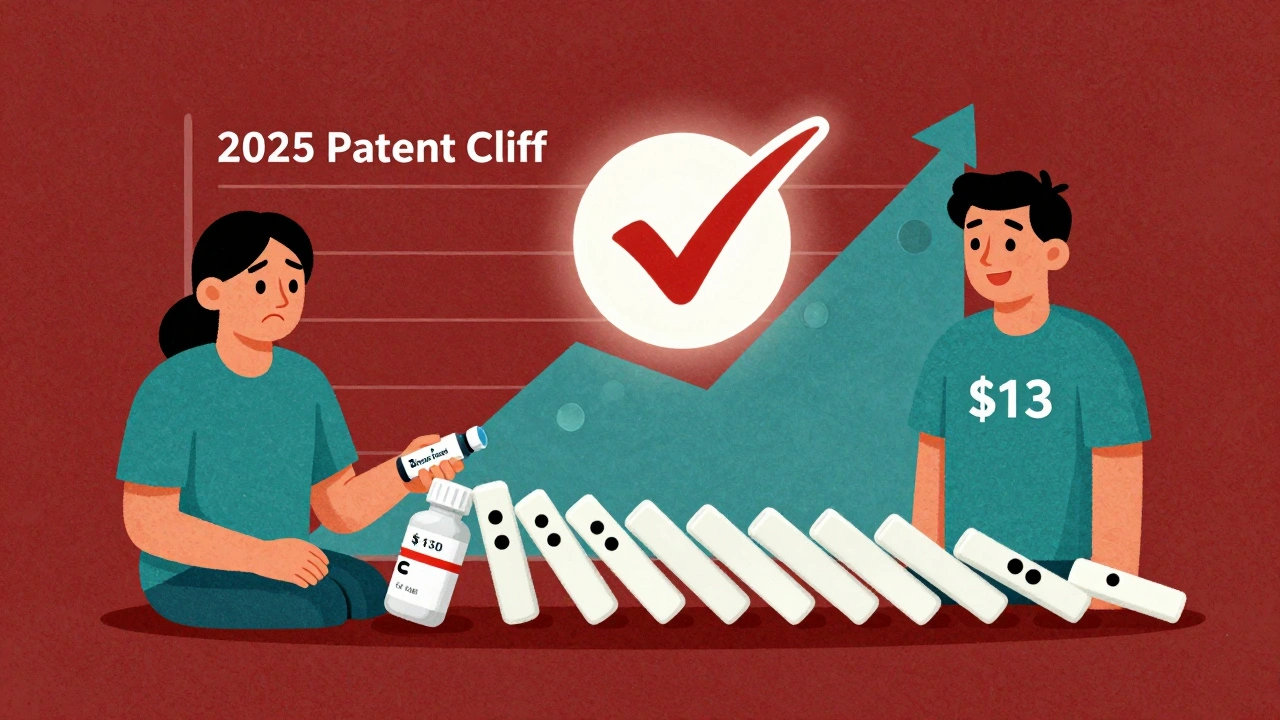
The average out-of-pocket cost for a generic prescription in 2024 was $6.95. For a brand-name drug? $28.69. That’s almost five times more. For someone on a fixed income, paying $7 instead of $29 every month adds up to over $260 saved in a year. For uninsured patients, the gap is even wider. Brand-name drug prices jumped 50% since 2019, hitting $130 per prescription on average. Meanwhile, generic prices dropped by 6% over the same period. That’s not inflation-it’s deflation in action.
The Numbers Behind the Market
The U.S. prescription drug market is worth $1.5 trillion. Without generics, that number would be closer to $2.7 trillion. That’s the gap between what we pay now and what we’d pay if every drug were brand-name. Since 2019, total spending on generics has actually gone down by $6.4 billion-even as more generics hit the market and prescriptions rose by 15%. That’s the power of competition. When multiple companies can make the same drug, prices don’t just drop-they collapse.
Take the 745 generic drugs approved by the FDA in 2024. Each one of those approvals meant at least one brand-name drug lost its monopoly. And it’s not just pills. Biosimilars-generic versions of complex biologic drugs like Humira and Enbrel-are now saving $20.2 billion a year. In oncology alone, biosimilars cut cancer drug spending growth in half since 2019. One cancer drug, Stelara, saw nine biosimilars enter the market by mid-2025. Prices dropped as much as 90%. That’s not a discount. That’s a revolution.
Why Do Brand Drugs Cost So Much?
It’s not because they’re better. It’s because they’re protected. Drug companies don’t just rely on patents-they build walls around them. A single blockbuster drug, for example, was granted over 75 patents to stretch its monopoly from 2016 all the way to 2034. That’s not innovation. That’s legal maneuvering. These are called “patent thickets.” They’re a tactic used to block generic companies from entering the market, even when the original patent expires.
Another trick is “product hopping.” That’s when a brand company slightly changes a drug-like switching from a pill to a liquid-and then files a new patent. Suddenly, the old version isn’t covered by insurance anymore, and patients are forced to pay full price for the new version, even if it does the exact same thing. The Congressional Budget Office estimates ending these practices would save $1.1 billion over ten years. That’s real money. Real people.

Who’s Using Generics-and Who’s Not?
Most Americans use generics without even thinking about it. Eighty-seven percent of commercial health plans now require pharmacists to substitute generics when available. Medicare beneficiaries are seeing massive savings too. For chronic conditions like psoriasis or Crohn’s disease, biosimilars have turned treatments that once cost $10,000 a year into options under $1,000.
But access isn’t equal. Only 42 states have updated their pharmacy laws to let pharmacists automatically switch a brand drug for a generic without asking the doctor first. In the other eight, patients and doctors have to jump through extra hoops-even when the FDA says the generic is just as safe and effective. That’s not healthcare policy. That’s bureaucracy.
Are Generics Really the Same?
Yes. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand. They must also be bioequivalent-meaning they work the same way in the body. The FDA tests them. They’re not copies. They’re approved equivalents.
Some patients worry about differences between generic manufacturers. There are over 150 companies making generics in the U.S. And yes, occasionally someone reports a change in how a drug feels after switching brands. But the FDA’s adverse event reports show these cases are rare-less than 1% of all generic prescriptions. For most people, switching from brand to generic makes no difference at all. For people with narrow therapeutic index drugs-like warfarin or levothyroxine-doctors may monitor levels more closely, but that’s standard practice, not a flaw in generics.
What’s Coming Next?
2025 is the year of the patent cliff. Three major drugs-Entresto, Tradjenta, and Opsumit-are losing patent protection. Together, they brought in $8.6 billion in sales last year. Once generics hit, prices will plummet. That’s $8.6 billion back in patients’ pockets and insurers’ budgets.
The FDA is approving generics faster than ever. In 2024, first-time generic approvals rose 12% from the year before. And new legislation is moving through Congress. The Affordable Prescriptions for Patients Act targets patent thickets. The Drug Competition Enhancement Act stops product hopping. Both have bipartisan support. If they pass, we’ll see even more savings.
Why This Matters
Generics aren’t just a cost-cutting tool. They’re a lifeline. For a diabetic paying $300 a month for insulin, switching to a generic version could mean choosing between medicine and groceries. For a heart patient on a fixed income, a $6 prescription instead of $30 means they won’t skip doses. For families, it means fewer medical bankruptcies.
The system isn’t perfect. Patent abuse is real. State laws are outdated. But the data doesn’t lie: generics deliver real, measurable, life-changing savings. They’ve saved $3.4 trillion over the last decade. They’re saving $445 billion a year. And with more patents expiring, more biosimilars launching, and more states updating their laws, the savings are only going to grow.
You don’t need to be a policymaker to benefit. The next time your doctor writes a prescription, ask: Is there a generic? If the answer is yes, you’re not just saving money. You’re helping fix a broken system-one prescription at a time.
Are generic drugs as safe and effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also meet strict bioequivalence standards, meaning they work the same way in the body. Generics go through the same manufacturing inspections and quality controls. Over 90% of prescriptions filled in the U.S. are generics, and adverse event reports show fewer than 1% involve issues tied to the generic version.
Why are generic drugs so much cheaper?
Generic manufacturers don’t have to repeat expensive clinical trials because they prove their drug is bioequivalent to the brand, not entirely new. That cuts development costs dramatically. Plus, once multiple companies start making the same drug, competition drives prices down. A drug that once cost $100 might drop to $5 or $10 after several generics enter the market. The savings come from efficiency and competition-not lower quality.
Can I ask my pharmacist to switch my brand drug to a generic?
In most cases, yes. Pharmacists are allowed to substitute a generic for a brand-name drug unless the doctor specifically writes “dispense as written” or “no substitution.” In 42 states, pharmacists can make the switch automatically without contacting the doctor. In the other eight, they may need to call first. Always check your state’s pharmacy laws, but don’t assume you’re stuck with the brand-ask your pharmacist.
Do insurance plans cover generics better than brand-name drugs?
Yes. Most insurance plans have lower copays for generics. Some even require you to try a generic first before covering the brand. Commercial health plans now mandate generic substitution in 87% of cases. Medicare Part D plans also have lower cost-sharing for generics. Even if you’re uninsured, many pharmacies offer generic drugs for under $10 through discount programs.
What’s the difference between a generic and a biosimilar?
Generics are exact copies of small-molecule drugs, like pills for blood pressure or cholesterol. Biosimilars are highly similar versions of complex biologic drugs-like injectables for arthritis, cancer, or autoimmune diseases. They’re not identical because biologics are made from living cells, not chemicals. But they work the same way and are proven safe and effective. Biosimilars have saved $56.2 billion since their introduction, with $20.2 billion saved in 2024 alone.
Will I save money if I switch from a brand drug to a generic?
Almost always. In 2024, the average out-of-pocket cost for a generic was $6.95. For a brand-name drug, it was $28.69. That’s a 76% savings. For drugs with multiple generics available, prices can drop even lower-sometimes under $5. If you’re paying $300 a month for a brand drug, switching to a generic could cut that by $200 or more. Ask your pharmacist or check GoodRx or SingleCare for current prices before filling your prescription.
Why don’t all doctors prescribe generics?
Many do-over 90% of prescriptions are for generics. But some doctors still default to brand names out of habit, lack of awareness, or because a patient had a bad experience with a generic in the past (which is rare). Some drug reps still visit offices and push brand-name products. If you’re concerned about cost, ask your doctor: “Is there a generic version available?” They’re usually happy to switch.
What’s the biggest barrier to more generic drug savings?
Patent thickets. Drug companies file dozens-even hundreds-of overlapping patents to delay generic entry. One drug extended its monopoly from 2016 to 2034 with 75 patents. This practice costs consumers $12 billion a year, according to Blue Cross Blue Shield. Until laws like the Affordable Prescriptions for Patients Act pass and are enforced, this loophole will keep blocking savings. The FDA and Congress are aware, but change moves slowly.



Ashley Skipp, December 11, 2025
Generics are lifesavers but nobody talks about how pharma bribes doctors to push brand names. I've seen it firsthand. The reps show up with free lunches and 'educational grants'-it's corruption dressed as medicine.
Robert Webb, December 12, 2025
It's fascinating how the economics here are so clear yet so ignored. When you have multiple manufacturers competing to make the same molecule, prices don't just drop-they implode. That's basic supply and demand, but the system is rigged to prevent that from happening too often. Patent thickets are essentially legal monopolies extended by paperwork. And product hopping? That's not innovation, that's fraud dressed up as R&D. The fact that we're still allowing this while people skip doses because they can't afford insulin is morally indefensible. We're not talking about luxury drugs here-we're talking about blood pressure pills, insulin, seizure meds. These aren't optional. They're survival. And yet, the system treats them like optional upgrades. The FDA does its job, pharmacists are ready, patients want it-but the gatekeepers? They're still holding the door shut with patent filings and lobbying dollars.
Rob Purvis, December 12, 2025
I love that biosimilars are finally gaining traction! I mean, Humira was costing over $70,000 a year before biosimilars came in-and now? It's under $10,000 in some places. That’s not just savings-that’s dignity restored. And the FDA’s approval process? Rock solid. I’ve worked in pharma compliance for 12 years, and the bioequivalence testing for generics is brutal-way stricter than most people realize. If your generic doesn’t hit 80–125% AUC and Cmax, it gets tossed. No exceptions. So when someone says, 'I feel different on the generic,' nine times out of ten, it’s psychological-or they switched between two different generics. The brand? It’s the same exact molecule. The packaging is just shinier.
Laura Weemering, December 14, 2025
I’ve been on levothyroxine for 15 years… and every time I switch generics, my TSH goes haywire… I’m not crazy. I’ve tracked it. The FDA says it’s fine, but my body says otherwise. Who are they to tell me how I feel? They don’t live in my skin. And don’t even get me started on the ‘corporate conspiracy’… Big Pharma, the FDA, the AMA-it’s all connected. You think they want you healthy? No. They want you dependent. On *their* version.
Stacy Foster, December 14, 2025
This whole post is a pharma shill. Did you know the FDA gets funding from drug companies? Yeah. They do. And the ‘bioequivalence’ standards? A joke. They test on 24 healthy college kids in Iowa. What about elderly diabetics with liver damage? Nobody cares. Generics are just cheap knockoffs with fillers that cause inflammation. I’ve seen people break out in rashes. The system is designed to kill slowly so you keep buying meds. Wake up.
Reshma Sinha, December 15, 2025
In India, generics are the backbone of healthcare. We have 50+ manufacturers of metformin. Price? $0.02 per tablet. Americans pay $28? That’s colonial economics. We need global solidarity on this. Pharma’s profit model is broken. It’s not about science-it’s about control.
Lawrence Armstrong, December 16, 2025
I’m a pharmacist in rural Ohio. I see this every day. Grandmas choosing between insulin and groceries. I switch them to generics without a second thought. Most don’t even notice the difference. And when they do? I give them a free sample of the brand to compare. 98% say the generic’s fine. 🤝💊
Donna Anderson, December 18, 2025
omg yes!! i switched my blood pressure med to generic and saved $200 a month. i started taking my dog to the vet more often bc i had the cash. also, my cousin’s kid with asthma? switched to generic inhaler. same results. no drama. why are we still paying brand prices??
Levi Cooper, December 19, 2025
This is why America is falling apart. We let foreign companies make our medicine. China controls 80% of the active ingredients. Our own FDA approves this? We’re literally outsourcing our health to authoritarian regimes. And you’re celebrating it? This isn’t savings-it’s surrender.
sandeep sanigarapu, December 20, 2025
Generics are the unsung heroes of global health. Simple, effective, affordable. The real issue is not the science, but the policy. Fix the laws, and the savings will follow.
Nathan Fatal, December 20, 2025
The deeper issue here isn’t just cost-it’s trust. We’ve been trained to equate price with quality. That’s a cultural conditioning, not a medical fact. When a drug costs $30, we assume it’s better. When it’s $7, we assume it’s weak. But the science doesn’t care about your perception. It only cares about bioequivalence. The real revolution isn’t in the pill-it’s in our minds. We need to stop worshiping brand names like they’re sacred relics and start treating medicine like what it is: a tool. And tools should be judged by function, not by logo.
nikki yamashita, December 20, 2025
this made me cry. my mom took generics for 10 years and never missed a dose. she’s 82 and still hiking. thank you for saying this.
Ashley Skipp, December 22, 2025
Exactly. And don’t get me started on how insurers still make you fail a brand first before covering the generic. Like, you have to go broke before you get help? That’s not healthcare. That’s punishment.