For people living with diabetes, managing blood sugar isn’t just about checking a number once a day. It’s about understanding how your body responds to food, stress, sleep, and medication - and making smart choices that keep you safe and healthy over the long term. Two tools stand at the center of this effort: A1C and daily glucose monitoring. One tells you where you’ve been over the past few months. The other shows you exactly what’s happening right now.
What A1C Really Tells You
A1C is a blood test that measures the percentage of your hemoglobin - the protein in red blood cells that carries oxygen - that’s coated with sugar. Since red blood cells live for about 120 days, the A1C result gives you a rolling average of your blood sugar over the last 2 to 3 months. It’s not a snapshot. It’s a story.
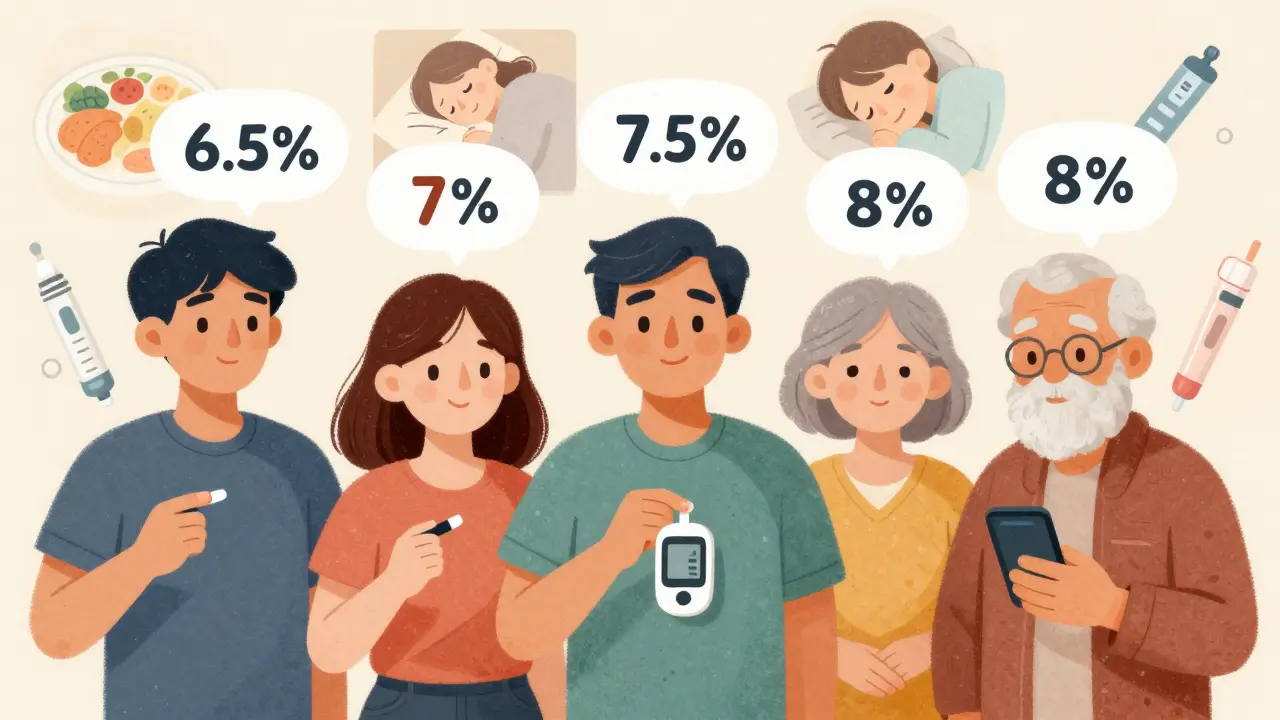
The American Diabetes Association (ADA) says most adults with diabetes should aim for an A1C below 7%. That’s about 154 mg/dL (8.6 mmol/L) average glucose. But here’s the catch: that number doesn’t work for everyone. A 75-year-old with heart disease and limited mobility might do better with a target of 8%. A 30-year-old with type 1 diabetes and no other health issues might safely aim for 6.5%.
Why the difference? Because tight control comes with risks. Lowering A1C too aggressively can lead to dangerous low blood sugar episodes - especially in older adults or people who don’t feel the warning signs. The ACCORD trial found that pushing A1C below 6% in some patients actually increased the risk of death. That’s not a typo. More medicine doesn’t always mean better outcomes.
In the UK, NICE guidelines recommend 6.5% for people newly diagnosed and on a single medication, and 7% for those on multiple drugs. Meanwhile, the American College of Physicians says 7-8% is appropriate for most people with type 2 diabetes. Why the split? Because real life isn’t a clinical trial. People have jobs, families, bills, and fears. A target that looks good on paper might be impossible to live by.
Daily Glucose Monitoring: Beyond the Fingerstick
If A1C is your history book, daily glucose monitoring is your live news feed. For decades, the only option was the fingerstick meter - pricking your finger, placing a drop of blood on a strip, waiting a few seconds for the number to appear. They’re cheap, widely covered by insurance, and still used by millions.
But they have limits. You get one number at a time. You don’t see the spikes after meals or the dips in the middle of the night. That’s where continuous glucose monitors (CGMs) come in. Devices like the Dexcom G7 and Abbott FreeStyle Libre 3 stick a tiny sensor under your skin that checks glucose in your interstitial fluid every 5 minutes. No more constant pricking. Just a quick scan or automatic sync to your phone.
CGMs don’t just show your current number. They show trends. You can see if your glucose is rising fast after pasta, dropping slowly during a walk, or creeping up overnight. That’s powerful. One user on Reddit said, “I finally understood why I felt shaky at 3 a.m. - my glucose was at 52. I had no idea until the CGM woke me up.”
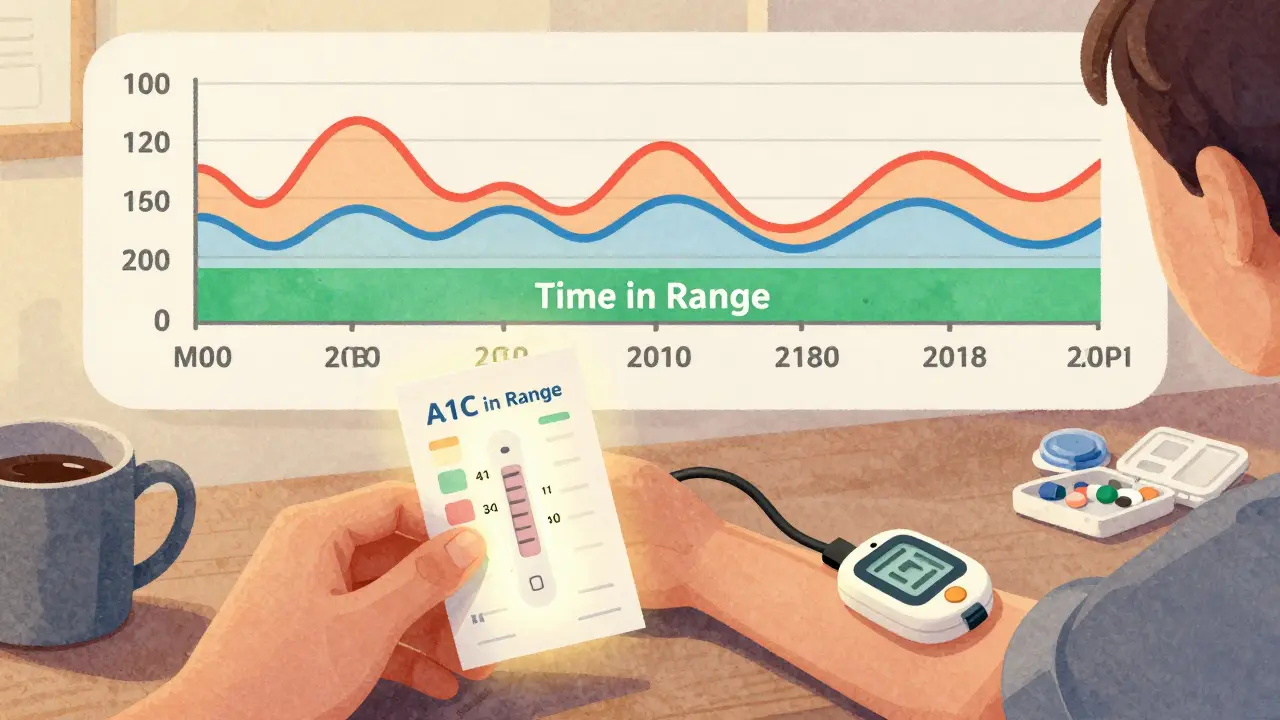
Modern guidelines now focus on “time in range” - the percentage of time your glucose stays between 70 and 180 mg/dL. The ADA recommends staying in range at least 70% of the day. That’s more useful than just an A1C number. Two people could both have an A1C of 7%, but one spends 90% of the day in range, while the other swings wildly between 40 and 250. Who’s at higher risk? The one with the wild swings.
Why A1C Isn’t Perfect
A1C is a great tool - but it’s not foolproof. If you have anemia, kidney disease, or certain hemoglobin variants (common in people of African, Mediterranean, or Southeast Asian descent), your A1C can be misleading. It might read lower than your actual average glucose, or higher. That’s not a test error. It’s biology.
Also, A1C doesn’t capture hypoglycemia. Someone could have a perfect 6.8% A1C but spend 2 hours a day below 60 mg/dL. That’s dangerous. And it’s invisible to the A1C test.
Even the way you test matters. A 2021 study found that 30% of home glucose meters give readings that are off by 10-15% because of poor technique, expired strips, or uncalibrated devices. If you’re relying on those numbers to make insulin decisions, you’re flying blind.
CGMs help fix this. They’re more accurate - especially at low glucose levels - and they don’t rely on user technique. But they’re expensive. In the U.S., out-of-pocket costs can hit $127 a month. Even with Medicare covering CGMs for insulin users since 2019, many people still ration strips or skip testing because they can’t afford it. A 2022 Health Affairs study found 32% of Medicaid patients cut back on test strips to save money. That’s not just inconvenient. It’s life-threatening.
Who Should Use What?
If you’re on insulin - whether type 1 or type 2 - a CGM is now considered standard care. The data is too valuable to ignore. You’ll catch lows before they happen. You’ll see how your lunch affects your afternoon. You’ll adjust faster and feel more in control.
If you’re on oral meds only and your blood sugar is stable, a fingerstick meter might be enough. Test before meals and at bedtime. That’s usually 4 times a day. But if you’ve had a low blood sugar episode, or if your A1C keeps creeping up despite “good” numbers, it’s time to consider a CGM.
Here’s a simple rule: if you’re afraid of low blood sugar, or if you don’t feel the symptoms when it happens, get a CGM. Hypoglycemia unawareness is silent, and it kills.
And if you’re newly diagnosed? Start with education. Don’t just get a meter and go. Work with a certified diabetes care specialist. Studies show that after 3 structured education sessions, 78% of people can recognize patterns in their glucose data. That’s the difference between guessing and knowing.
How Often Should You Test?
There’s no one-size-fits-all answer. But here’s what most experts agree on:
- If you’re on insulin: test 4-10 times a day, or use a CGM.
- If you’re on oral meds and stable: test 1-2 times daily, maybe before breakfast and after dinner.
- If you’re changing medications or diet: test more often - at least 3-4 times daily for 2 weeks to see patterns.
- A1C testing: every 3 months if your treatment is changing or you’re not meeting targets. Twice a year if you’re stable.
Medicare covers 100 test strips a month for insulin users. For non-insulin users, it’s only 100 strips every 3 months. That’s often not enough. If you’re struggling, ask your doctor for a letter of medical necessity. Many insurers will approve more if you can show you’re using the data to prevent complications.

The Real Challenge: Stress, Cost, and Burnout
Managing diabetes isn’t just about numbers. It’s about mental health. A 2023 survey found that 68% of people with diabetes feel anxious about their A1C results before clinic visits. Some call it “A1C denial” - avoiding testing because they’re scared of bad numbers.
Others feel overwhelmed. “I’m tired of being a lab rat,” one user wrote. “I just want to eat without calculating.” That’s valid. Diabetes burnout is real. And pushing someone to hit a 6.5% A1C when they’re exhausted, underpaid, and working two jobs isn’t care - it’s cruelty.
Dr. Rebecca Bensen-Kennedy from the American College of Physicians put it bluntly: “A one-size-fits-all approach ignores the heterogeneity of diabetes patients and may cause more harm than good.”
That’s why personalized goals matter. Your target should match your life. Your age. Your health. Your resources. Your fears. If you’re 70, live alone, and have no family nearby, your target shouldn’t be the same as a 35-year-old with a support system and a tech-savvy partner.
What’s Next? The Future of Monitoring
Technology is moving fast. Google and Dexcom are working on a contact lens that measures glucose - no sensors, no sticks. It’s not here yet, but it’s coming. By 2025, we could see non-invasive options entering the market.
Hybrid closed-loop systems - like Tandem’s Control-IQ - are already doing the work for you. They adjust insulin automatically based on CGM data. Real-world data shows they increase time in range by 12% and lower A1C by half a point.
But tech alone won’t fix this. The biggest barrier isn’t the device. It’s access. Only 22% of type 2 diabetes patients use CGMs, compared to 74% of type 1 patients. Why? Cost. Insurance. Lack of awareness. And yes - racism and poverty. People of color and low-income communities are far less likely to get these tools, even when they’re medically needed.
The ADA’s 2024 initiative is trying to fix that. They’re building algorithms that factor in social determinants - income, housing, food access - when setting targets. That’s progress.
Final Takeaways
- A1C tells you your average blood sugar over 3 months - but it doesn’t show the highs and lows.
- Time in range (70-180 mg/dL) is now just as important as A1C. Aim for 70% or more.
- CGMs are better than fingersticks for spotting trends and preventing lows.
- Your A1C target should be personal. 7% isn’t a law. 8% might be safer - and more realistic.
- Testing frequency depends on your treatment. Insulin users need more data. Others can test less.
- Cost and mental health are huge barriers. Don’t let perfection stop you from progress.
Diabetes management isn’t about hitting a number. It’s about living well. The goal isn’t a perfect A1C. It’s fewer hospital visits. Better sleep. More energy. Less fear. And the tools - whether a meter, a CGM, or a conversation with your doctor - are there to help you get there, not punish you for falling short.



Hakim Bachiri, December 28, 2025
A1C below 7%? LOL. My uncle’s been at 6.2% for 8 years, and he’s had three hypoglycemic seizures. You want perfect numbers? Fine. But don’t act like it’s some moral victory when your blood sugar’s so low you can’t remember your kid’s name. #DiabetesIsNotAClub
Gran Badshah, December 29, 2025
in india, most people just check once a week because strips cost more than a meal. we dont have access to cgms, and insurance? haha. my mom uses a 5-year-old meter that sometimes gives 200 when it's 90. she still tries. that's the real story.
Ellen-Cathryn Nash, December 30, 2025
I just want to say… I’m *so* tired of people treating diabetes like a video game where you level up by hitting a number. You’re not a robot. You’re a human being who’s trying to survive a system that doesn’t care if you’re exhausted, broke, or grieving. Your worth isn’t measured in mg/dL. And if your doctor says ‘7% or else’? Find a new one. 🙄
Samantha Hobbs, December 31, 2025
i got my first cgm last year and holy crap it changed my life. i used to think i was fine because my a1c was 7.1… then i saw i was dipping to 54 every night at 2am. no symptoms. no warning. just… falling asleep. now i eat a snack before bed. simple. life-saving. why isn’t this covered for everyone?
Nicole Beasley, January 2, 2026
time in range = 70%? 🤯 i didn’t even know that was a thing! i’ve been staring at my a1c like it’s a report card. but now i’m obsessed with my cgm trends… i’m at 78%! 🎉 i finally feel like i’m not just surviving. i’m living. 🙌
sonam gupta, January 4, 2026
why do americans act like diabetes is a luxury problem? we have people here who use one strip a week and guess the rest. your cgms and algorithms dont mean anything when you’re choosing between insulin and rent
Julius Hader, January 4, 2026
I’ve been a type 2 for 15 years. I’ve had my A1C at 6.9, 7.3, 7.8… and I’m still here. Alive. Working. Cooking for my grandkids. The number isn’t the point. The fact that I’m not in the hospital? That’s the win. Don’t let anyone make you feel guilty for living your life.
Vu L, January 5, 2026
So let me get this straight… we’re now supposed to believe that a 7% A1C is *too* aggressive, but CGMs are the holy grail? But only if you can afford $127/month? And the real solution is… not forcing people to be perfect? That’s the big reveal? Wow. Groundbreaking.
James Hilton, January 5, 2026
A1C is a myth. CGMs are the truth. But the real villain? The system that lets Big Pharma charge $127 for a sensor while people die because they can’t afford to test. We need healthcare, not hype. And yes, I’m from the US. And I’m embarrassed.