When you’re pregnant, every pill, supplement, or over-the-counter medicine feels like a potential risk. You’re not just thinking about yourself anymore-you’re thinking about the tiny life growing inside you. And that’s why medication safety during pregnancy matters more than ever. But here’s the hard truth: most of the drugs you might take while pregnant haven’t been properly tested on pregnant women. Not because they’re dangerous, but because they’ve never been studied in that group. That leaves a massive gap in what doctors and patients actually know.
Why Pregnancy Medication Safety Is So Complicated
For decades, drug labels used simple letters-A, B, C, D, X-to tell you if something was safe during pregnancy. It sounded straightforward. But it wasn’t. Many women saw a “C” and assumed it meant “dangerous,” so they stopped taking their blood pressure meds, antidepressants, or thyroid pills. Turns out, those letters didn’t measure risk-they just said how much data existed. And in most cases, there wasn’t enough. In 2015, the FDA got rid of the letter system. It replaced it with detailed, plain-language sections in drug labels: Pregnancy, Lactation, and Females and Males of Reproductive Potential. Now, instead of guessing what a letter meant, you get real info: what animal studies showed, what human data exists, and what the risks might be. But here’s the catch-only about 1 in 10 drugs have enough human data to give you a clear answer. A 2020 study in JAMA Network Open found that between 2003 and 2012, only 5-10% of FDA-approved drugs had solid evidence on how they affected fetuses. That means for the other 90%, doctors are making educated guesses. And that’s terrifying when you’re the one holding the prescription.What Happens When You Stop Your Medication
The fear of harm often leads women to stop essential medications. But stopping can be just as dangerous as taking them. A 2021 survey by the American Academy of Family Physicians found that 68% of obstetricians regularly see patients who’ve stopped needed meds because they were scared. One woman stopped her antidepressants when she got pregnant. Within weeks, she was in crisis-severe anxiety, panic attacks, insomnia. She didn’t know that untreated depression carries higher risks for preterm birth, low birth weight, and developmental delays than most antidepressants. The American College of Medical Toxicology says it plainly: No medication is 100% safe during pregnancy. But untreated medical conditions can be even riskier. High blood pressure, diabetes, epilepsy, asthma, mental health conditions-these don’t just disappear when you get pregnant. If left unmanaged, they can lead to preeclampsia, stillbirth, or lifelong complications for your child. A study from Massachusetts General Hospital tracked 12,500 pregnant women and found that after the FDA dropped the letter system, inappropriate medication discontinuation dropped by 18%. Why? Because women started getting real information, not confusing labels. That’s progress. But it’s not enough.The System That’s Supposed to Protect You
Both the U.S. and Europe have systems in place to track medication use during pregnancy. The FDA runs 38 active pregnancy exposure registries. These are voluntary programs where women who take certain drugs during pregnancy sign up and get followed through delivery and beyond. The goal? To collect real-world data so we can learn faster. But here’s the problem: less than 1% of all pregnant women taking medications ever enroll in these registries. Dr. Christina Chambers from UC San Diego found that safety alerts are delayed by an average of 7.2 years because we’re not collecting data fast enough. That’s seven years of women taking drugs with unknown risks, while researchers wait for enough cases to emerge. In Europe, the EMA requires drug companies to monitor pregnancy exposure for medications with known or suspected fetal risks. For drugs like lenalidomide (used to treat multiple myeloma), they require mandatory pregnancy testing and birth control for six months after treatment ends. It’s strict. But a 2022 European audit found that 41% of companies didn’t even meet the minimum requirements. And here’s another gap: only 28% of U.S. hospitals have electronic systems that can automatically flag a pregnant patient’s medication list and warn doctors about potential risks. That means most safety checks still rely on a doctor remembering to ask, “Are you taking anything else?”
What You Should Do Right Now
You don’t need to wait for perfect data. You need a plan. At your first prenatal visit, bring every medication you take. That includes prescriptions, OTC painkillers, herbal teas, vitamins, CBD oil, and supplements. ACOG recommends a full medication reconciliation-this takes about 22 minutes, but it’s one of the most important things you’ll do in your pregnancy. Check the label. Look for the “Pregnancy” section. It’s no longer a letter. It’s a paragraph. It might say: “No adequate human studies,” or “Animal studies show fetal harm,” or “Data from over 1,500 exposed pregnancies show no increased risk.” Don’t skip it. Don’t stop without talking to your provider. If you’re on a medication and you’re worried, don’t quit cold turkey. Talk to your OB, your pharmacist, or call a specialized hotline like Mass General’s Pregnancy Medication Safety Line. They handled over 12,000 calls in 2022-and 78% of those calls ended with the recommendation to keep taking the medication. Take folic acid. 800 mcg daily, starting before conception and continuing through at least 12 weeks. It reduces the risk of neural tube defects by up to 70%. It’s one of the few things with rock-solid evidence. Avoid known dangers. Isotretinoin (Accutane) for acne? Absolutely not. It causes severe birth defects in 20-35% of exposed pregnancies. Valproate for seizures? Avoid unless there’s no alternative-it raises neural tube defect risk from 0.1% to 1-2%. Thalidomide? Never. These aren’t “maybe” risks. These are clear, proven dangers.Where to Find Reliable Info (And Where Not to)
Reddit’s r/Bump has over a million members. It’s full of stories, fears, and advice. But 68% of posts there complain about conflicting or unclear information. One woman wrote: “My doctor told me to stop my antidepressant. Now I’m having withdrawal and panic attacks. Why isn’t there clearer guidance?” Drugs.com had 1.8 million pregnancy-related queries in 2022. Forty-two percent of negative reviews said the info was contradictory. That’s not helpful. Stick to trusted sources: the FDA’s “Medicine and Pregnancy” page, the CDC’s pregnancy medication guides, or the American College of Obstetricians and Gynecologists (ACOG). Healthline’s review of the FDA’s pregnancy page gave it 4.3 out of 5 stars. One user wrote: “The section on cannabis risks helped me decide to stop CBD. I didn’t know it could affect my baby’s brain development.”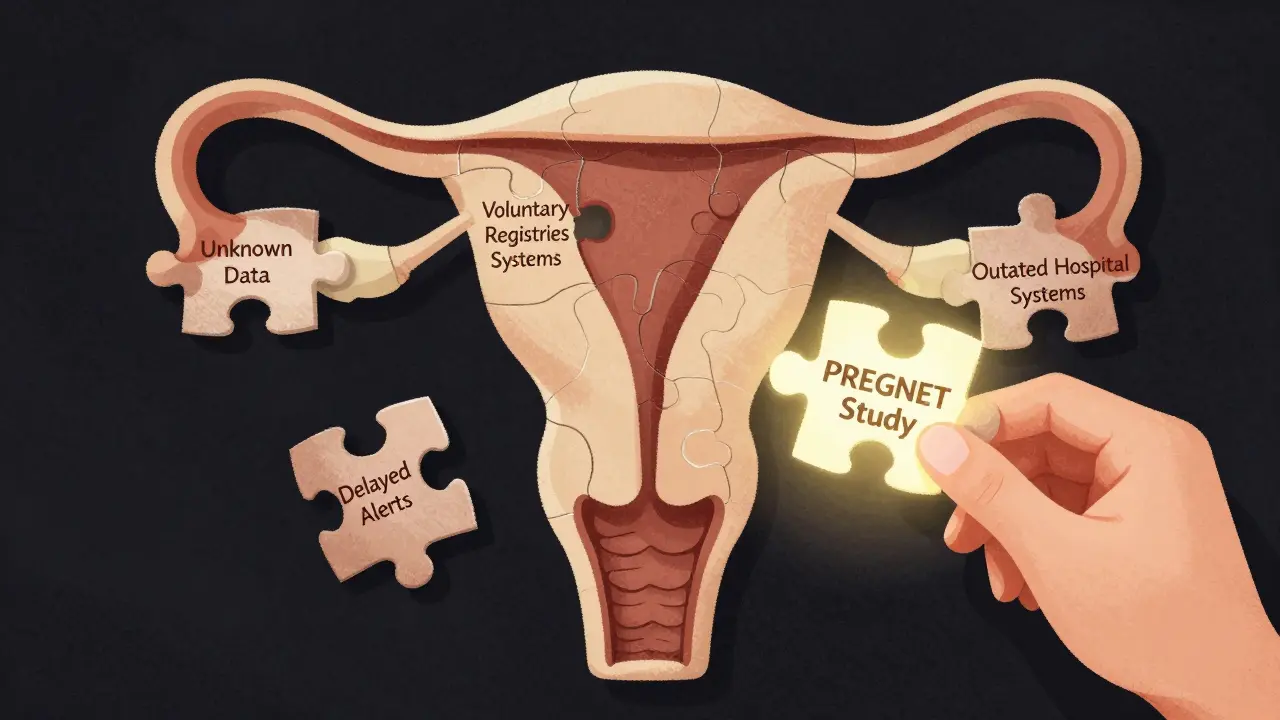




Alex Warden, January 2, 2026
This whole thing is a scam. The FDA doesn't care about moms, they care about drug profits. They let companies test on animals, then slap a 'C' on it and sell it to us like it's fine. I stopped all meds when I got pregnant-no way I'm letting Big Pharma poison my kid. If you're taking antidepressants or blood pressure pills, you're playing Russian roulette. 🤬
LIZETH DE PACHECO, January 2, 2026
I just want to say thank you for writing this. I stopped my thyroid med because I was scared, and I ended up in the ER with extreme fatigue and panic attacks. My OB helped me get back on it safely. You're right-stopping can be worse. Please, if you're scared, talk to someone. You don't have to do this alone. 💛
Lee M, January 4, 2026
The real issue isn't the drugs-it's the collapse of epistemic authority. We've replaced medical expertise with algorithmic noise and fear-based social media narratives. The FDA's old letter system was flawed, yes-but the new system doesn't fix the core problem: society has outsourced critical thinking to corporate-funded data streams. We're not just misinformed-we're epistemically disoriented.
Bryan Anderson, January 5, 2026
I appreciate the thorough breakdown. One thing I’d add is that pharmacists are often underutilized resources. Many don’t realize that pharmacists can review all your meds-prescription, OTC, supplements-and give you a pregnancy-specific risk assessment. I work at a hospital pharmacy, and we’ve started offering free 15-minute consults for expectant parents. It’s simple, free, and way more reliable than Googling at 2 a.m.
Matthew Hekmatniaz, January 6, 2026
As someone who grew up in a culture where pregnancy means total abstinence from all meds, I used to think this was about being ‘natural.’ But after seeing my sister nearly lose her baby from uncontrolled diabetes, I realized it’s not about avoiding pills-it’s about managing health. We need to stop shaming women for taking meds and start supporting them with real data. Everyone deserves to be informed, not terrified.
Liam George, January 7, 2026
You think this is about safety? Nah. This is about population control. The FDA, WHO, and Big Pharma are all in bed with the same shadowy elites pushing birth control through medication fear. They don’t want you to have healthy babies-they want you to be dependent on their ‘safe’ drugs while quietly sterilizing the population with endocrine disruptors in your ‘essential’ meds. The 7-year delay in safety alerts? That’s not negligence. That’s intentional. Wake up. The registry? A trap. Don’t sign up. Don’t trust the labels. Your baby’s DNA is worth more than their corporate compliance.
sharad vyas, January 9, 2026
In India, many women take nothing during pregnancy because they believe it’s better to suffer than to risk a pill. But my aunt had severe asthma and still carried two healthy kids-because her doctor helped her use the right inhaler. No magic. Just science. We need more stories like this, not fear. Simple truth: care is better than silence.
Dusty Weeks, January 9, 2026
folic acid 800mcg is the only thing that matters. everything else is noise. 🙏💊