Getting vaccinated while on immunosuppressants isn’t just about when you get the shot-it’s about whether it works at all. If you’re taking medication for rheumatoid arthritis, lupus, cancer, or an organ transplant, your immune system is already working under heavy restrictions. A vaccine given at the wrong time might as well be a placebo. The difference between a strong immune response and no protection at all often comes down to a few weeks-or even months-of timing.
Why Timing Matters More Than You Think
Most people assume vaccines work the same way for everyone. But if you’re on drugs like rituximab, methotrexate, or cyclophosphamide, your body’s ability to build immunity is slowed down, sometimes drastically. Studies show that people on B-cell depleting therapies like rituximab can have up to a 90% lower antibody response to mRNA vaccines if vaccinated too soon after treatment. That’s not just a small drop-it’s the difference between being protected and being vulnerable. The goal isn’t just to get the vaccine. It’s to get it when your immune system has the best shot at responding. That means coordinating with your doctor to pause or delay your immunosuppressant medication, not just for convenience, but for survival.Key Rules by Medication Type
Not all immunosuppressants are the same. Some hit your immune system hard and fast. Others are slower but steady. Here’s what the latest guidelines say, broken down by drug class:- Rituximab (and other B-cell depleters): Wait at least 6 months after your last dose before getting any vaccine except flu. Some experts say 9 months is safer. Why? These drugs wipe out the very cells that make antibodies. Even if you wait 3 months, your body might still be too empty to respond. The CDC and IDSA agree: don’t rush this.
- Methotrexate: This one’s a rare exception where timing actually makes a big difference. Hold it for two weeks after your flu shot or COVID booster. Studies show this boosts antibody levels by 27%. You can usually keep taking it for other vaccines, but for flu and COVID, those two weeks matter.
- TNF inhibitors (like adalimumab or etanercept): Pause for one dose before vaccination, then wait four weeks after to restart. This gives your immune system a brief window to react without triggering a disease flare.
- Mycofenolate, azathioprine, leflunomide: You can usually keep taking these for non-live vaccines. But if you’re getting a live vaccine (like shingles or MMR), stop them for four weeks before and after. Live vaccines can be dangerous if your immune system is too suppressed.
- IVIG (intravenous immunoglobulin): The dose matters. If you got 1 gram per kilogram of body weight, wait 10 months before a live vaccine. For lower doses, it’s still 8 months. This isn’t a suggestion-it’s a requirement. IVIG contains antibodies that can neutralize the vaccine before it even has a chance to work.
When to Get Vaccinated Before Starting Treatment
If you’re about to start immunosuppressants-maybe because you’ve just been diagnosed with an autoimmune disease or are preparing for chemotherapy-the best time to get vaccinated is before you take your first pill. The CDC recommends at least 14 days before starting treatment. But many specialists, especially in oncology and rheumatology, push for 4 to 6 weeks. Why? Because it takes time for your body to build up antibodies. A 2023 study in Journal of Clinical Oncology found that patients vaccinated 6 weeks before chemo had antibody levels nearly double those vaccinated just two weeks prior. For people with cancer, this is often easier to plan. Your oncologist will schedule your chemo around your vaccine dates. But for autoimmune patients, it’s trickier. You might be waiting months for a rheumatology appointment. Don’t wait. If you know you’re going to need immunosuppressants, ask your doctor about getting your vaccines now-even if your disease isn’t flaring yet.
What About Live Vaccines?
Live vaccines-like MMR, varicella (chickenpox), and the nasal flu spray-contain weakened versions of the virus. They’re great for healthy people. But for someone on immunosuppressants, they can be risky. The rule is simple: Don’t get live vaccines while on immunosuppressants unless your doctor says it’s safe. Even if you’re on a low dose, the risk isn’t worth it. If you need a live vaccine, you must stop your medication for at least four weeks before and after. And even then, your doctor might still say no. For people on rituximab or similar drugs, live vaccines are often off the table entirely. That’s why it’s critical to get them before you start treatment. If you missed that window, talk to your doctor about alternatives. There’s a non-live shingles vaccine (Shingrix) that’s just as effective and completely safe for immunocompromised patients.Real Problems Real People Face
Guidelines sound clear on paper. In real life? They’re messy. At Massachusetts General Hospital, 42% of patients on rituximab had to wait six months for their shingles vaccine. During that time, 18% got shingles anyway. One patient wrote on a patient forum: “I waited six months. Got the shot. Got shingles two weeks later. My doctor said it was ‘just how it is.’ But I didn’t feel like I was given a real choice.” Others struggle with disease flares. When you stop methotrexate for two weeks to get a flu shot, your joint pain might come roaring back. Your rheumatologist might say, “It’s temporary.” But if you’re already in pain, waiting two weeks feels like torture. And then there’s the coordination problem. Most patients see a rheumatologist, a primary care doctor, and maybe an oncologist. None of them always talk to each other. A 2023 survey found that 47% of family doctors didn’t know how to time vaccines for patients on immunosuppressants. That means you’re often the one who has to ask the right questions.What’s Changing in 2025?
The old model-“wait 6 months, then get the shot”-is starting to break down. New research is pointing toward something smarter: personalized timing based on your immune system’s actual state. The NIH is running a study called VAXIMMUNE, tracking 2,500 people to see if measuring B-cell counts or antibody levels can tell us exactly when to vaccinate. Early results suggest that if your B-cells are above 50 cells per microliter, you’re likely ready for a vaccine-even if it’s only been 3 months since your last rituximab dose. Hospitals are also building tools. Epic Systems, the big electronic health record company, is rolling out a vaccine timing calculator in 2025. It will automatically check your meds, your last dose dates, and your vaccine history-and tell your doctor the best window to schedule your shot. This isn’t science fiction. It’s the future. And it’s coming fast.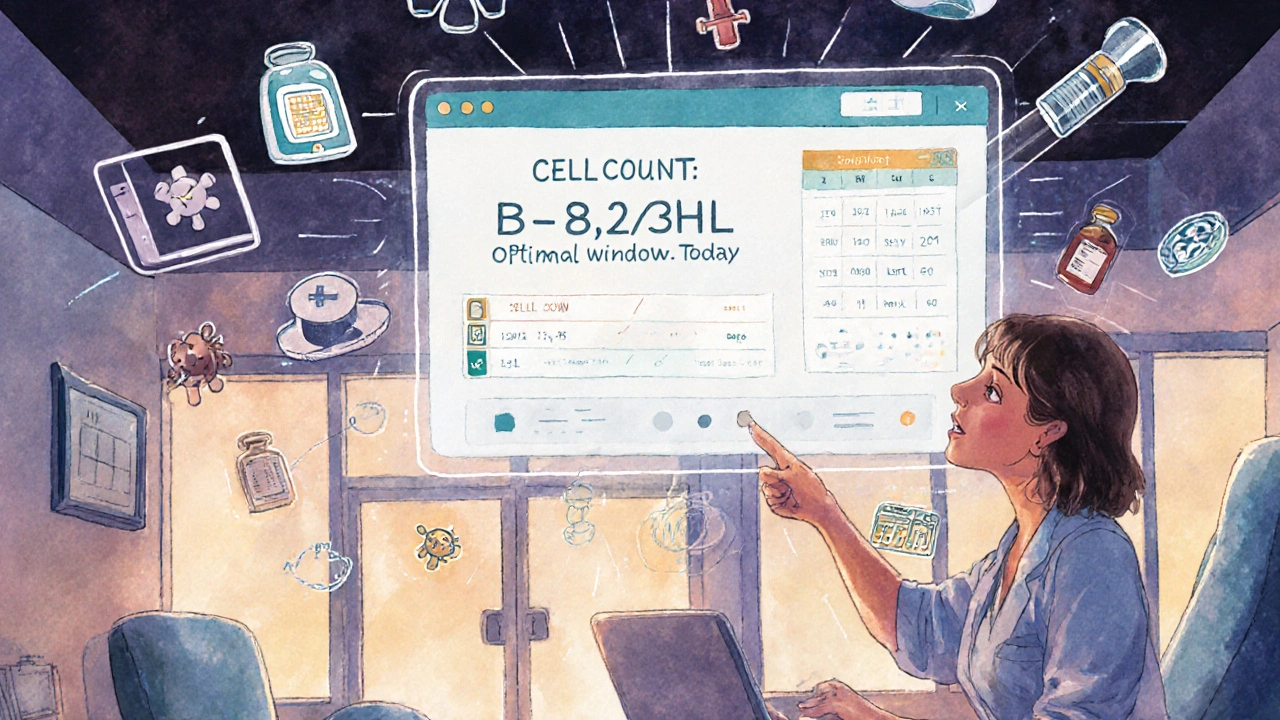
What You Should Do Right Now
If you’re on immunosuppressants, here’s your action plan:- Make a list of every medication you take. Include doses and when you last took them.
- Check which vaccines you’ve had. Did you get the flu shot this year? The shingles vaccine? The updated COVID booster?
- Call your doctor. Don’t wait for your next appointment. Say: “I need to know the safest time to get my next vaccine based on my current meds.”
- Ask if you can get a blood test. Specifically: “Can we check my B-cell count or antibody levels?” This could change your timeline.
- Don’t assume your pharmacist or primary care doctor knows. Immunology is complex. Your specialist needs to be involved.
Frequently Asked Questions
Can I get the flu shot while on methotrexate?
Yes, you can. But holding methotrexate for two weeks after the shot increases your immune response by nearly 30%. If your arthritis is under control, ask your doctor if you can pause it temporarily. If you’re having a flare, they may advise you to keep taking it-your health comes first.
How long after rituximab should I wait for the COVID vaccine?
Wait at least 6 months after your last rituximab dose. Some experts recommend waiting 9 months, especially if you’re high-risk. Studies show antibody levels rise sharply after this point. Getting it too early often gives you no protection at all.
Can I get vaccinated if I’m on IVIG?
Yes, but timing depends on your dose. For a 1 g/kg dose, wait 10 months before a live vaccine. For non-live vaccines like flu or COVID, you can usually get them after 3 months. IVIG contains antibodies that can block the vaccine’s effect, so waiting is critical.
What if I missed the window before starting immunosuppressants?
It’s not ideal, but it’s not hopeless. You can still get vaccinated after starting treatment, but your response will likely be weaker. Ask your doctor about getting a booster after your immune system has had time to recover. Some patients benefit from extra doses-especially for COVID and flu.
Are there any vaccines I should avoid completely?
Avoid live vaccines like MMR, varicella, and the nasal flu spray while on immunosuppressants. They can cause infection in people with weakened immune systems. Stick to inactivated or mRNA vaccines-these are safe and effective.
Why do some doctors say to wait 2 weeks and others say 6 months?
Different drugs affect the immune system in different ways. For most medications, 2-4 weeks before is enough. But for B-cell depleters like rituximab, the damage lasts much longer. That’s why guidelines vary. Always ask which drug you’re on and how it works-not just what the rule is.




Emily Entwistle, November 19, 2025
Yesss!! This is exactly why I made my rheumatologist hold my methotrexate before my last booster 😌💉 I was skeptical but my antibody test came back through the roof! Who knew two weeks of joint pain was worth it? 🤗 #VaccineTimingWins
Gregory Gonzalez, November 20, 2025
How quaint. You’re all acting like this is groundbreaking news. I’ve been telling my patients since 2018 that rituximab patients are essentially immunological ghosts. The fact that you need a CDC guideline to understand that antibodies don’t magically appear in a vacuum… well, it’s almost charming in its naivety. 🥂
Ronald Stenger, November 21, 2025
Forget the science-this is why America’s healthcare system is crumbling. You’ve got people waiting six months for a vaccine because some bureaucrat in a lab coat says so. Meanwhile, China’s giving booster shots to everyone within 72 hours of chemo. We’re out here playing chess while they’re playing Fortnite. Get it together.
Samkelo Bodwana, November 21, 2025
Let me tell you something from Cape Town-this isn’t just an American problem. My cousin in Johannesburg is on azathioprine and got shingles last year because her clinic didn’t know about the four-week rule. We don’t have Epic Systems. We don’t even have consistent electronic records. The real issue isn’t timing-it’s access. If you’re poor, rural, or in a developing country, these guidelines might as well be written in Sanskrit. We need systems, not just lists.
Duncan Prowel, November 22, 2025
While the clinical guidelines presented are largely consistent with current IDSA and CDC recommendations, one must acknowledge the methodological limitations of the cited studies-particularly the small sample sizes in B-cell reconstitution cohorts. Furthermore, the assertion that IVIG neutralizes vaccine antigens requires clarification: it is not a universal phenomenon, but rather dose- and time-dependent, with variable IgG half-lives across individuals. A more granular analysis of pharmacokinetics is warranted before universal protocols are applied.
Bruce Bain, November 24, 2025
So… if you’re on medicine that kills your immune system, wait before you get the shot. And if you haven’t gotten the shot yet, get it before you start the medicine. And if you’re on IVIG, wait even longer. And don’t get the nasal spray. Got it. Simple. Why does this feel so complicated? 😅
Jonathan Gabriel, November 25, 2025
Okay, so let me get this straight-science says we should time vaccines based on B-cell counts, but most docs don’t even know what a B-cell is? And we’re waiting for Epic to build a calculator because human beings can’t read a chart? 🤦♂️ I’m not mad, I’m just disappointed. We’ve got AI that can predict stock markets but can’t tell a rheumatologist when to vaccinate their patient? This isn’t medicine. It’s a glitch in the matrix. Typo: 'immunosuppresants'-but you get the point.
Don Angel, November 25, 2025
Thank you for this. Seriously. I’ve been scared to ask my doctor anything because I don’t want to sound dumb. But this? This made me feel like I’m not alone. I’m on adalimumab, and I just called my PCP and asked them to coordinate with my rheum doc. I’m nervous, but I’m doing it. Thank you for giving me the words to say.
benedict nwokedi, November 27, 2025
Wait… so you’re telling me the government and Big Pharma are letting us get vaccines at random times… while they know exactly when they should be given? And they’re not telling us? And now they’re rolling out a ‘calculator’? That’s not innovation-that’s damage control. They’ve been lying about efficacy for years. They knew. They’ve always known. This is just another cover-up wrapped in a white coat. Check your blood. Check your mind. Don’t trust the system.
deepak kumar, November 28, 2025
Bro, this is gold. I’m from Delhi and my uncle is on methotrexate-he got his flu shot without pausing, and he’s fine! But now I’m going to tell him to hold it for two weeks. Also, don’t forget: in India, we don’t have access to antibody tests. So we do what we can. This info? It’s a lifeline. Thank you for writing this so clearly. 🙏
Dave Pritchard, November 29, 2025
If you’re reading this and you’re on immunosuppressants-please don’t feel guilty for asking questions. Your life matters more than a doctor’s schedule. You’re not being difficult. You’re being smart. And if your doctor rolls their eyes? Find a new one. You deserve care that sees you as a person, not a chart.
kim pu, November 30, 2025
Okay but what if the whole vaccine thing is just a psyop to sell more drugs? Like, what if the ‘low antibody response’ is manufactured? I mean, why do they even need to time it? Why not just pump us full of antibodies? Why not just give us the real stuff? This feels like a trap. Also, I think my shingles came from 5G towers. Just saying. 😈
malik recoba, December 1, 2025
my doc told me to wait 6 months after rituximab but i got my flu shot at 4 months and nothing happened. i’m not saying it’s safe, but… maybe it’s not as bad as they say? i’m just saying. maybe we’re all too scared to try anything? typos: 'immunosuppresants' again lol
Sarbjit Singh, December 2, 2025
Bro, this post saved my life. I’m on mycofenolate and was gonna get the shingles shot next week. Now I’m calling my doctor to pause it for 4 weeks. You’re right-this info isn’t out there. We need more posts like this. 🙏❤️
Emily Entwistle, December 2, 2025
@malikrecoba I’m so glad you’re being careful!! But please don’t skip the 4-week pause for live vaccines-your risk of getting infected from the vaccine is real. I had a friend who got the nasal flu spray and ended up in the ER. It’s not worth it. Stick to Shingrix. It’s the MVP. 💪🩹