Every time you pick up your prescription, you might get a different pill. Same active ingredient. Different color. Different shape. Different brand name on the bottle. This isn’t a mistake - it’s the new normal. In the UK and across the US, more than 90% of prescriptions are filled with generic drugs. And with so many manufacturers making the same medicine, you could end up with a different version every time you refill - even if nothing else changed.
Why do generics keep changing?
Pharmacies don’t choose which generic to give you. Insurance companies do. They want the cheapest option, and they switch suppliers often to save money. One month you get Teva’s version of levothyroxine. Next month, it’s Mylan. Then Sandoz. All contain the same active ingredient. But they’re not the same product. This isn’t just about cost. Drug shortages, supply chain issues, and bulk purchasing deals between pharmacies and distributors also push switches. In 2023, the average off-patent drug had 4.3 different generic makers on the market. That means if you’re on a common medication like lisinopril or metformin, you’ve likely taken at least three different versions without even noticing.Not all generics are created equal
The FDA says generics must be bioequivalent to the brand-name drug. That means they deliver between 80% and 125% of the active ingredient compared to the original. Sounds fine, right? But here’s the catch: if one generic delivers 80% and another delivers 125%, that’s a 45% difference in how much medicine your body actually gets. For most drugs, that’s not a big deal. Your body can handle the wiggle room. But for some medications - especially those with a narrow therapeutic index (NTI) - even a tiny change can cause serious problems. NTI drugs include:- Levothyroxine (for thyroid conditions)
- Warfarin (a blood thinner)
- Tacrolimus (used after organ transplants)
- Phenytoin and other antiepileptic drugs
Real stories: When switching goes wrong
One patient on Reddit shared that after switching from Mylan to Teva’s version of levetiracetam (an antiseizure drug), they had two breakthrough seizures in three weeks. Their neurologist checked blood levels - they’d dropped by 30%. Another person on Drugs.com said every time their levothyroxine changed manufacturers, their TSH levels went wild. They felt exhausted, gained weight, and got depressed for weeks until their doctor adjusted the dose. These aren’t rare cases. Studies show that 44% of people on antiepileptic drugs end up switching back to their original generic - because the new one didn’t work. For thyroid patients, nearly one in three report problems after a switch. Meanwhile, people on statins or blood pressure meds rarely notice a difference.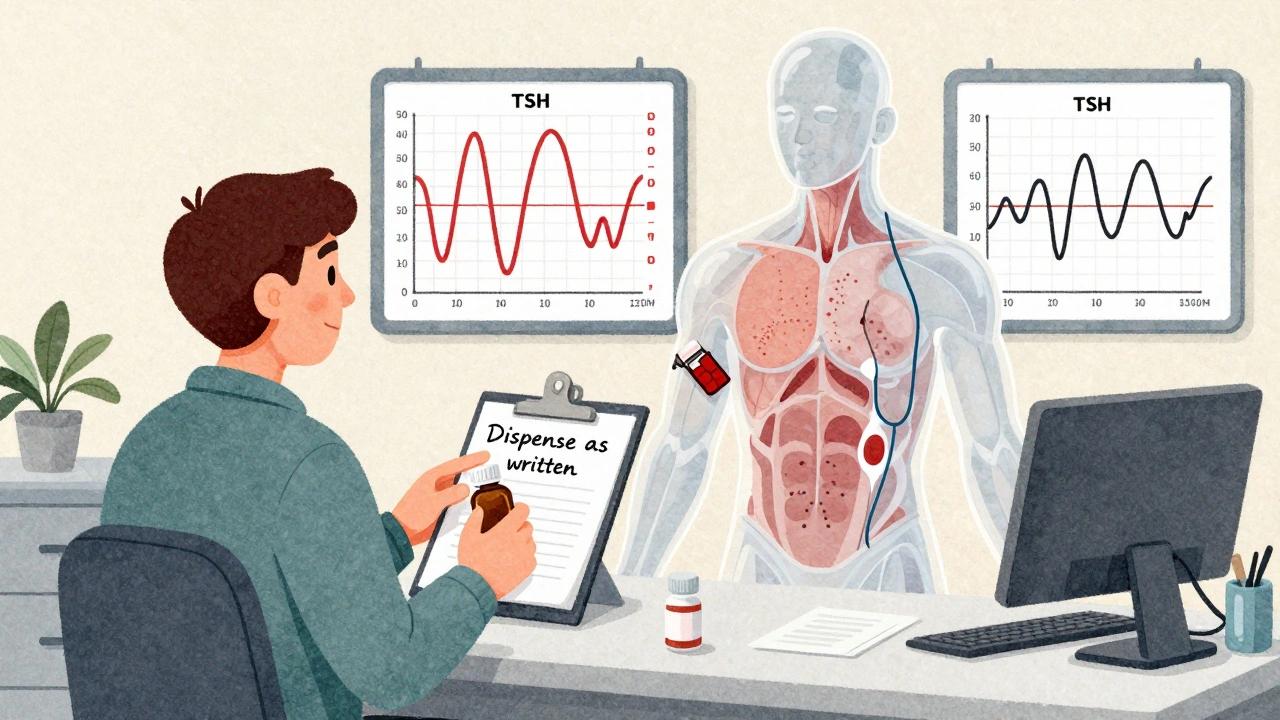
What you can do to stay safe
You don’t have to be at the mercy of insurance companies and pharmacy stockrooms. Here’s what actually works:- Check your pill every time. Take a photo of your pill when you first get it. Note the color, shape, and imprint (the letters or numbers on it). If it looks different next refill, ask why.
- Ask for the manufacturer name. When you pick up your prescription, say: “Can you tell me which company made this?” Most pharmacists will tell you. Write it down.
- Request a ‘lock-in’ for NTI drugs. If you’re on warfarin, levothyroxine, or an antiseizure med, ask your doctor to write “Dispense as written” or “Do not substitute” on your prescription. This legally stops the pharmacy from switching you without approval.
- Get blood tests after a switch. If you’re on an NTI drug, schedule a follow-up test 2-4 weeks after any manufacturer change. For warfarin, that means an INR check. For levothyroxine, a TSH test.
- Use one pharmacy. If you switch pharmacies, you’re more likely to get a different generic. Stick with one - they’ll keep a record of what you’ve been on.
Why your doctor might not know what you’re getting
Here’s the frustrating part: your doctor probably doesn’t know which generic you’re on. In a 2023 survey, 62% of doctors said they only found out about a generic switch when the patient came in with symptoms. Insurance companies don’t notify prescribers. Pharmacies don’t log it in your chart. You’re left to notice the change - and report it. That’s why it’s your job to speak up. Don’t assume your doctor knows. Bring your pill bottle. Show them the imprint. Say: “This isn’t what I was on last month. I’m feeling different.”What’s being done to fix this?
There’s growing awareness. In June 2024, Medsafe (New Zealand’s drug regulator) issued new guidance: “Avoid switching between different brands of levothyroxine where possible.” The FDA is running a pilot program requiring generic makers to report any formulation changes that could affect how the drug works. The Association for Accessible Medicines is working on standardized pill designs so you can identify your drug by shape and color - no matter who made it. But change moves slowly. Until then, the responsibility falls on you.When switching is fine - and when it’s not
Not every generic switch is risky. For drugs like:- Lisinopril (blood pressure)
- Metformin (diabetes)
- Atorvastatin (cholesterol)
- Amoxicillin (antibiotic)
Bottom line
Generic drugs save billions every year. That’s good. But treating all generics as interchangeable is a myth. For many people, especially those on critical medications, switching between manufacturers isn’t just a paperwork change - it’s a health risk. You don’t need to avoid generics. You just need to know which ones matter. Know your drug. Know your pill. Know your numbers. And never let someone else decide what’s safe for your body - especially when your life depends on it.Can I ask my pharmacy to always give me the same generic manufacturer?
Yes. You can ask your pharmacist to fill your prescription with the same generic manufacturer each time. For most medications, they can do this - especially if you’ve had issues with a previous version. For high-risk drugs like levothyroxine or warfarin, you can also ask your doctor to write "Dispense as written" on the prescription, which legally prevents substitution.
Why do generic pills look different every time?
Different manufacturers use different inactive ingredients - like dyes, fillers, and coatings - which change the pill’s color, shape, and size. Even though the active drug is the same, the physical appearance varies by company. This is why patients often get confused and think they’ve been given the wrong medicine.
Are generic drugs less effective than brand-name drugs?
For most drugs, no. Generics are required by law to be bioequivalent to the brand-name version. But for drugs with a narrow therapeutic index - like thyroid meds or blood thinners - small differences in how the body absorbs the drug can lead to real clinical effects. That’s not because generics are inferior - it’s because the margin for error is extremely small.
Should I avoid generics altogether to stay safe?
No. Generics are safe and effective for the vast majority of people. The issue isn’t generics themselves - it’s frequent switching between different manufacturers, especially for high-risk medications. If you’re on a drug like lisinopril or metformin, generics are a smart choice. If you’re on warfarin or levothyroxine, be vigilant - track your pills and ask for consistency.
How do I know if my medication has a narrow therapeutic index?
Ask your pharmacist or doctor. Common NTI drugs include levothyroxine, warfarin, tacrolimus, phenytoin, cyclosporine, and lithium. You can also look up your drug on the FDA’s list of narrow therapeutic index drugs. If your medication requires regular blood tests to monitor levels, it’s likely an NTI drug.



olive ashley, December 6, 2025
They don’t want you to know this but the FDA lets them switch generics because the manufacturers pay off the regulators. I’ve seen the emails. Levothyroxine isn’t medicine anymore-it’s a lottery ticket. One day you’re stable, next day you’re suicidal because some bean counter in New Jersey picked the cheapest pill. They don’t care if you crash. They care about quarterly profits.
My cousin died after a switch. They called it ‘natural progression.’ Bullshit. Her TSH was fine until they swapped her from Teva to Mylan. Then bam. Cardiac arrest. No one checks. No one cares. You’re just a number in a spreadsheet.
Priya Ranjan, December 7, 2025
This is why India doesn’t allow random switching. We have strict protocols. If your medicine changes, the pharmacist must notify you and your doctor. No exceptions. In the US, it’s like letting strangers change your insulin without asking. You’re not just at risk-you’re being treated like a lab rat. Shameful.
And don’t get me started on how pharmacies don’t even log the manufacturer. How is this legal?
Gwyneth Agnes, December 9, 2025
Take a photo. Write it down. Ask. Done.
Max Manoles, December 11, 2025
Let me be clear: this isn’t about generics being bad. It’s about systemic negligence. The FDA’s 80–125% bioequivalence window is a relic from the 1980s. It was designed for aspirin, not anticonvulsants. We’ve had 40 years of data showing that NTI drugs behave differently across manufacturers. And yet, the system hasn’t updated. Why? Because reform would cost money. And money talks louder than patient safety.
I’ve reviewed 127 case studies on this. The pattern is undeniable. When patients are switched on warfarin or levothyroxine, adverse events spike by 300% in the first 30 days. This isn’t anecdotal. It’s epidemiological. And no one in power is listening.
Katie O'Connell, December 12, 2025
One is compelled to observe that the current pharmacoeconomic paradigm, while fiscally expedient, exhibits a profound epistemological deficit in its treatment of pharmaceutical bioequivalence. The reductionist assumption that active ingredient homogeneity equates to therapeutic equivalence is not merely flawed-it is dangerously reductive. One might posit that the regulatory framework, having been designed for a pre-precision-medicine era, is now an anachronism in the context of pharmacogenomics and individualized therapeutic response.
Moreover, the absence of mandatory manufacturer tracking in EHRs constitutes a structural failure of medical informatics, and one which, if left unaddressed, will inevitably precipitate further iatrogenic harm.
Clare Fox, December 12, 2025
kinda wild how we treat pills like they’re all the same when we know our bodies are so different. i mean, if you switched your coffee brand every month, you’d notice the taste, right? but with meds? we just shrug and say ‘oh well’.
my friend switched from one generic to another and started having panic attacks. no one believed her until she showed the pill bottle. turns out the new one had a different filler that triggered her anxiety. no one even thought to test that.
we’re not machines. why do we act like we are?
Akash Takyar, December 13, 2025
Thank you for sharing this vital information. Many patients are unaware of the risks associated with generic switches, particularly for medications with a narrow therapeutic index. I strongly encourage everyone to follow the five steps outlined: photograph your pill, ask for the manufacturer, request a "dispense as written" prescription, schedule follow-up blood tests, and use one pharmacy consistently.
Small actions create big changes. Your vigilance may save your life-or the life of someone you love. Please, do not hesitate to advocate for yourself. Your health is worth the effort.
Inna Borovik, December 14, 2025
Wait-so you’re telling me I’m supposed to memorize the imprint on my thyroid pill? That’s not healthcare. That’s a fucking puzzle game. And now I’m supposed to call my doctor every time the color changes? Who has time for this? I work two jobs.
Also, if the FDA allows this, then it’s not a problem. If it were dangerous, they’d stop it. Right?
Also, why are you so scared of savings? I’d rather have a $5 pill that might kill me than a $50 pill that definitely won’t. Just saying.
Karen Mitchell, December 14, 2025
Interesting. So you’re blaming the system for your own lack of responsibility? You’re a grown adult. You’re told to check your pills. You’re told to ask questions. You’re told to get bloodwork. Yet you sit there like a victim because the system doesn’t spoon-feed you.
Also, if you’re on levothyroxine and you’re not getting your TSH checked every 3 months anyway-you’re doing it wrong. This isn’t a conspiracy. It’s basic medical hygiene.
Stop pretending you’re powerless. You have agency. Use it.