When antidepressants don’t work, what’s next? For many people struggling with depression, anxiety, or chronic pain, the answer isn’t just another pill-it’s a different kind of medicine. SNRI medications offer a powerful alternative when first-line treatments like SSRIs fall short. Unlike SSRIs that target only serotonin, SNRIs work on two key brain chemicals: serotonin and norepinephrine. This dual action makes them especially useful for people who feel mentally foggy, exhausted, or physically aching alongside their low mood.
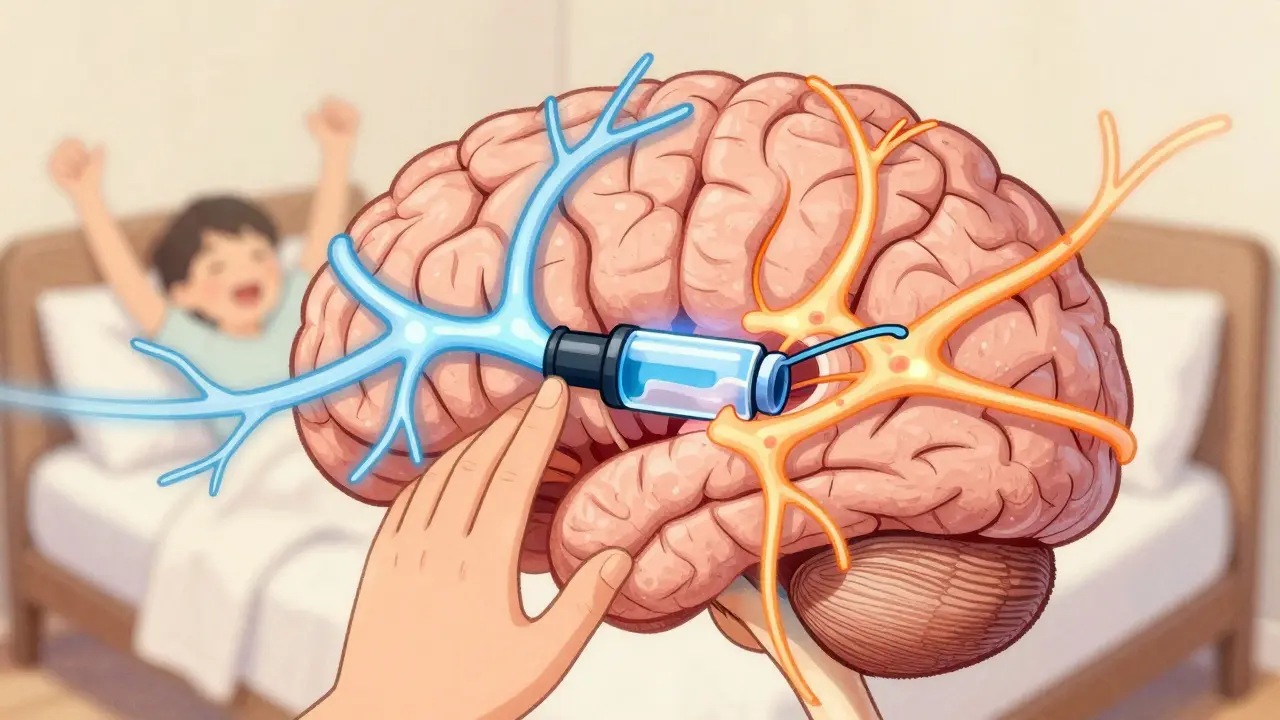
How SNRIs Actually Work
SNRIs stand for Serotonin and Norepinephrine Reuptake Inhibitors. That’s a mouthful, but here’s what it means in plain terms: your brain uses serotonin and norepinephrine to regulate mood, energy, focus, and even pain signals. After these chemicals do their job, they’re usually pulled back into nerve cells-like a vacuum sucking up leftover crumbs. SNRIs block that vacuum. That means more serotonin and norepinephrine stay active in the spaces between brain cells, helping signals flow better.
This isn’t just theory. Real people notice the difference. Someone with depression who feels too tired to get out of bed might find themselves able to walk the dog again after a few weeks on duloxetine. A person with fibromyalgia who’s been told their pain is ‘all in their head’ might finally get real relief from nerve pain that’s lasted years.
Not all SNRIs work the same way. Venlafaxine (Effexor XR), for example, acts mostly like an SSRI at low doses (under 75mg), but kicks in as a true SNRI at higher doses (150mg+). Duloxetine (Cymbalta), on the other hand, hits both chemicals from day one. That’s why doctors often choose duloxetine for patients with both depression and chronic pain-it’s built for both.
Which SNRIs Are Approved and Used Today
In the U.S., four SNRIs are FDA-approved for treating depression:
- Venlafaxine (Effexor XR) - The first SNRI approved back in 1993. Still widely used, especially for treatment-resistant depression.
- Duloxetine (Cymbalta, Drizalma Sprinkle) - Not just for depression. Also approved for diabetic nerve pain, fibromyalgia, and chronic back pain. The only SNRI approved for pediatric anxiety in 2022.
- Desvenlafaxine (Pristiq) - A metabolite of venlafaxine. Often prescribed for patients who had side effects with Effexor.
- Levomilnacipran (Fetzima) - Known for boosting energy and focus more than others. Often chosen when fatigue is a major symptom.
These aren’t just for depression. Duloxetine is one of the few antidepressants with official approval for chronic pain. That’s huge. For people with osteoarthritis or nerve pain from diabetes, it’s not a side benefit-it’s the main reason they’re taking it.
How Long Does It Take to Work?
Don’t expect miracles in a week. SNRIs, like most antidepressants, take time. Most people start noticing small improvements around week 4-better sleep, less crying spells, a bit more motivation. But real change? That usually shows up between weeks 6 and 12. Some people need the full 12 weeks before they feel like themselves again.
That’s why quitting too early is so common-and so risky. Many stop because they don’t feel better right away, or because the nausea hits hard in the first few days. But that nausea? It usually fades after 10-14 days. The same goes for dizziness or dry mouth. The body adjusts.
Doctors always start low and go slow. A typical first dose might be 37.5mg of venlafaxine XR once a day, then increased every week or two. Jumping to a high dose too fast can spike blood pressure or cause severe nausea. Patience isn’t optional-it’s part of the treatment.

Side Effects: What to Expect
No medication is without trade-offs. SNRIs are generally better tolerated than older antidepressants like tricyclics, but they’re not gentle. Here’s what most people experience:
- Nausea - Affects about 25% of people on duloxetine. Usually mild and short-lived.
- Dizziness - Especially when standing up quickly. Happens in 15-20% of users.
- Insomnia or sleepiness - Depends on the person. Some feel wired; others feel drugged.
- Sexual side effects - Lowered libido, trouble reaching orgasm. Reported by 20-30% of users.
- Blood pressure rise - A real concern. About 5-8% of users develop high blood pressure that needs monitoring.
- Withdrawal symptoms - If you stop suddenly, you might get ‘brain zaps,’ flu-like symptoms, or severe anxiety. This affects 20-30% of people who quit cold turkey.
Here’s the thing: these side effects are worse in the first few weeks. Many people stop because they think it’s the medication-not the adjustment. But if you stick with it, most side effects shrink or disappear. And if they don’t? Your doctor can lower the dose or switch you to another SNRI.
SNRIs vs. SSRIs: What’s the Real Difference?
SSRIs like sertraline (Zoloft) or escitalopram (Lexapro) are still the first choice for depression. Why? They’re gentler. Fewer side effects. Easier to start.
But SNRIs have a clear edge in two areas:
- Energy and focus - If you’re stuck in a fog, lethargic, unable to concentrate, SNRIs often help more than SSRIs. Levomilnacipran and venlafaxine are especially strong here.
- Pain relief - For nerve pain, fibromyalgia, or chronic back pain, SNRIs are often the best drug option. SSRIs? Not so much.
A 2022 study showed that duloxetine reduced pain by 30-50% in 40-50% of patients with diabetic neuropathy. Placebo? Only 20-30% saw any reduction. That’s not a small win-it’s life-changing for people who’ve been told nothing can help their pain.
For pure depression without pain? The difference between SNRIs and SSRIs is small. Studies show SNRIs might be 5-10% more effective, but not dramatically so. That’s why doctors don’t start with them unless there’s a reason-like fatigue, lack of response to SSRIs, or physical symptoms.
Who Benefits Most from SNRIs?
SNRIs aren’t for everyone. But they’re perfect for specific profiles:
- People who tried one or two SSRIs and saw no improvement.
- Those with depression plus chronic pain (nerve pain, arthritis, fibromyalgia).
- Patients who feel mentally sluggish, tired, or unmotivated-more than just sad.
- People with anxiety disorders who also have physical symptoms like muscle tension or headaches.
- Adults or teens with generalized anxiety disorder (especially since duloxetine got pediatric approval in 2022).
It’s also worth noting: SNRIs work better when paired with therapy. A 2022 trial found that 73% of people who took an SNRI + cognitive behavioral therapy (CBT) went into remission. Only 48% did with medication alone. Therapy isn’t optional-it’s force multiplier.
What Happens When You Stop?
Stopping an SNRI suddenly is like flipping a light switch off in a dark room. You don’t just go dark-you get flashes, dizziness, nausea, and electric shock-like sensations (called ‘brain zaps’). These aren’t dangerous, but they’re awful.
The fix? Taper slowly. A 2021 study showed that tapering over 4-6 weeks cut withdrawal symptoms from 28% down to just 9%. That’s a massive difference. Never quit cold turkey. Even if you feel fine, keep taking it until your doctor says it’s safe to reduce.
And here’s a hard truth: 32% of people stop SNRIs because of side effects. Only 18% stop because they didn’t work. That means most people quit not because it failed-but because the side effects felt worse than the depression.
Cost, Availability, and Future Trends
In 2022, SNRIs made up 28% of all antidepressant prescriptions in the U.S. Venlafaxine and duloxetine alone accounted for 28% of the market. Generic versions are widely available and affordable. A 30-day supply of generic venlafaxine can cost under $10 with insurance-or even less with discount programs like GoodRx.
The future? More precision. Researchers are now using genetic tests to see how your body metabolizes SNRIs. If you have a CYP2D6 gene variant, you might process venlafaxine too slowly-leading to side effects. Testing can help avoid trial-and-error.
New combos are also being tested. One Phase III trial combined duloxetine with esketamine (a nasal spray used for treatment-resistant depression) and saw remission in 45% of patients-up from 28% with SNRI alone. That’s promising.
And digital tools? A 2023 study found that pairing duloxetine with a cognitive training app improved memory and focus by 35% more than the drug alone. Technology isn’t replacing meds-it’s making them better.
Final Thoughts: Is an SNRI Right for You?
If you’ve tried SSRIs and still feel stuck-tired, in pain, foggy-SNRIs might be the next step. They’re not magic. They come with side effects. They take time. But for the right person, they can be the bridge back to a normal life.
Don’t give up after one failed medication. Antidepressants aren’t one-size-fits-all. Sometimes it’s not that the drug doesn’t work-it’s that you haven’t found the right one yet. SNRIs are a proven, powerful option for those who need more than serotonin alone.
Work with your doctor. Track your symptoms. Be patient. And don’t let fear of side effects stop you from trying something that could finally help.
Are SNRIs better than SSRIs for depression?
SNRIs aren’t clearly better for depression alone. SSRIs are still first-line because they have fewer side effects. But SNRIs can be more effective for people with depression plus fatigue, low energy, or chronic pain. If an SSRI didn’t help, an SNRI might be the next step.
Can SNRIs help with chronic pain?
Yes. Duloxetine and venlafaxine are FDA-approved for diabetic nerve pain, fibromyalgia, and chronic musculoskeletal pain. Studies show 40-50% of patients get at least 30-50% pain reduction. For many, this is the first real relief they’ve had in years.
How long do SNRI side effects last?
Most side effects-like nausea, dizziness, or insomnia-peak in the first 1-2 weeks and fade as your body adjusts. Sexual side effects and blood pressure changes may last longer and need monitoring. If side effects are unbearable after 4-6 weeks, talk to your doctor about adjusting the dose or switching.
Do SNRIs cause weight gain?
Unlike some antidepressants, SNRIs don’t usually cause significant weight gain. Some people even lose a little weight at first due to nausea or reduced appetite. Long-term weight changes vary by person, but SNRIs are generally considered weight-neutral compared to medications like paroxetine or mirtazapine.
Can teens take SNRIs?
Yes. Duloxetine (Cymbalta) received FDA approval for pediatric generalized anxiety disorder in 2022. It’s the only SNRI currently approved for use in teens. All antidepressants carry a black box warning for increased suicidal thoughts in people under 25, so close monitoring is required during the first few months.
What should I do if I want to stop taking an SNRI?
Never stop abruptly. Work with your doctor to create a slow taper plan-usually over 4-6 weeks. Stopping suddenly can cause brain zaps, dizziness, nausea, and anxiety. A gradual reduction cuts withdrawal risk from nearly 30% down to under 10%.



Harry Henderson, January 28, 2026
SNRIs saved my life after 3 years of SSRIs doing nothing. I was a zombie. Now I run 5Ks and actually remember my kids' birthdays. Stop whining about nausea - it’s a week of suffering for a decade of clarity.
Kegan Powell, January 30, 2026
man i just think about how our brains are these messy little electrical storms and these pills are like whispering to the storm to calm down 🌩️💙
no magic just chemistry trying to be kind
April Williams, January 31, 2026
Why is everyone acting like SNRIs are some miracle cure? My cousin went on Cymbalta and turned into a rage monster who cried during commercials. This isn’t treatment - it’s chemical manipulation with a side of corporate greed.
Kathy McDaniel, January 31, 2026
i just started venlafaxine last week and honestly i feel a lil more awake?? like i can hear birds again 😅 maybe it’s placebo but i’ll take it
Desaundrea Morton-Pusey, February 1, 2026
Big Pharma’s new toy. They’ll sell you anything if it has a patent. SSRIs are fine. You just need to suck it up and get therapy. This is just another cash grab.
Murphy Game, February 1, 2026
Ever wonder why all these meds have the same side effects? They’re all made by the same 3 companies. The FDA’s just rubber-stamping. Brain zaps? That’s your nervous system screaming for help - not withdrawal. They don’t want you to know that.
John O'Brien, February 3, 2026
Levomilnacipran is the real MVP for brain fog. I was stuck in mud for 18 months. 2 weeks on Fetzima and I finished a book. No cap. Side effects? Yeah, but worth it. Don’t let fear stop you.
suhail ahmed, February 3, 2026
in india we call this 'chemical yoga' - you're not fighting your brain, you're just giving it a new rhythm 🌿
my uncle took duloxetine for diabetic pain and now dances at weddings again. no joke. medicine isn't the enemy - silence is.
Candice Hartley, February 4, 2026
My mom’s been on Cymbalta for 5 years. Pain gone. Sleep better. Still has dry mouth but she says it’s a small price. I’m so glad she didn’t quit after week 2.
astrid cook, February 5, 2026
People don’t realize how dangerous this is. You’re not fixing depression - you’re masking it with synthetic neurotransmitters. What happens when you’re 70 and your brain forgets how to make serotonin on its own?
Andrew Clausen, February 5, 2026
Correction: Duloxetine is not approved for pediatric anxiety. It’s approved for generalized anxiety disorder in adolescents 7 and older. The FDA label explicitly excludes children under 7. Stop misrepresenting data.
Anjula Jyala, February 7, 2026
SNRIs inhibit SERT and NET with high affinity but pharmacokinetics vary based on CYP2D6 polymorphisms which explains interindividual variability in response and adverse events especially with venlafaxine
Kirstin Santiago, February 8, 2026
I know someone who tried SNRIs and it didn’t work for them - but then they started yoga and journaling and now they’re thriving. Not saying meds are bad but sometimes the quiet stuff matters too.
you don’t have to choose one or the other.
Paul Taylor, February 9, 2026
Look I’ve been on three different SNRIs over 8 years and I’ve got a whole notebook on this. First I did venlafaxine - nausea so bad I threw up every morning for 10 days but then it clicked. Then duloxetine for fibro pain - worked like a charm but gave me night sweats. Then pristiq because I couldn’t handle the blood pressure spikes. Each one had a different flavor. The key is not to give up after the first bad week. Your body needs to learn the new rhythm. And yeah the brain zaps when you quit cold turkey? Brutal. I tapered over 10 weeks. Felt like walking through molasses but I didn’t lose my mind. Also therapy was the real game-changer. The pill just gave me the energy to show up for it. Don’t let fear or bad advice stop you from finding what works. You’re not broken. You’re just waiting for the right key.
Conor Murphy, February 11, 2026
My brother took Cymbalta after years of therapy failed. He said it didn’t make him happy - but it made him able to care again. That’s the difference. Not euphoria. Just… presence. 🫂
Harry Henderson, February 13, 2026
And to the person who said ‘Big Pharma’ - if you think your therapist is giving you free pills, you’re delusional. They’re not getting paid to push meds. They’re getting paid to watch you suffer longer. Get real.