Antiplatelet Therapy Risk Calculator
Risk Assessment
Personalized Recommendations
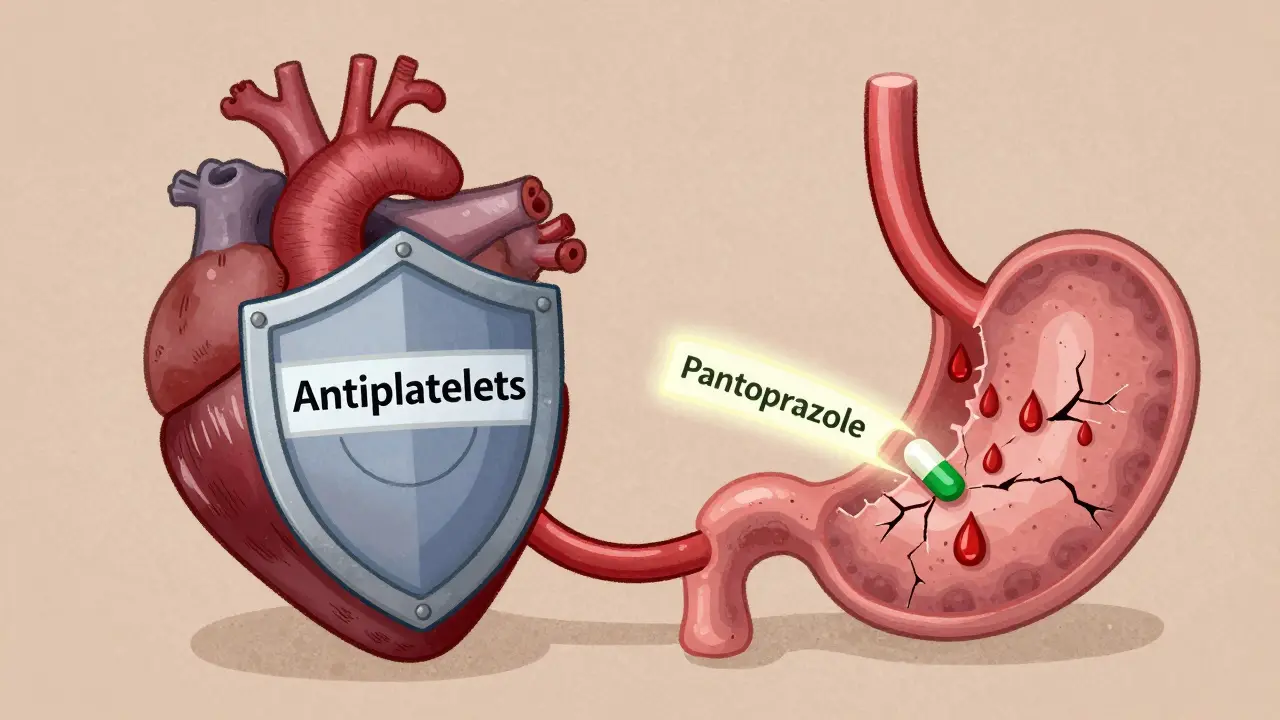
When you’re on dual antiplatelet therapy - usually aspirin plus clopidogrel, prasugrel, or ticagrelor - your blood doesn’t clot as easily. That’s good for preventing heart attacks and strokes. But it also means your stomach is more vulnerable. Every year, thousands of people on these medications end up in the hospital with dangerous gastrointestinal (GI) bleeding. The good news? There’s a proven way to cut that risk without weakening your heart protection: adding a proton pump inhibitor (PPI).
Why GI Bleeding Is a Real Danger on Antiplatelets
Aspirin alone can double your risk of a stomach bleed. Add another antiplatelet like clopidogrel, and that risk jumps by 30% to 50%. This isn’t theoretical. In the first 30 days after starting dual therapy, three out of every 100 patients will have a major GI bleed. Most of these happen silently - no warning, no pain - until they collapse from internal bleeding. The problem isn’t just the drugs. Age, prior ulcers, NSAID use, or being on blood thinners like warfarin make it worse. If you’re over 65 and on aspirin and clopidogrel after a stent, your risk isn’t just higher - it’s dangerous. And unlike a heart attack, GI bleeds don’t come with an EKG or a troponin test. By the time you feel dizzy or vomit blood, you’re already in crisis.How PPIs Actually Work (And Why They’re Not Just Antacids)
PPIs like omeprazole, esomeprazole, and pantoprazole don’t just calm heartburn. They shut down the acid pumps in your stomach lining - the same ones that make stomach acid. When these pumps are blocked, your stomach stays less acidic. That’s critical because blood clots need a certain pH to form. Less acid means clots form faster and stick better to damaged tissue, helping stop bleeding before it starts. Studies show PPIs cut major GI bleeds by 34% to 37%. In one trial with nearly 100,000 stroke patients on dual therapy, those taking a PPI had a 37% lower chance of a serious bleed over a year. That’s not a small benefit. It’s life-saving. And it works whether you’re on low-dose aspirin (81 mg) or higher doses - the protection holds up.The Big Catch: Omeprazole Can Hurt Your Heart Protection
Here’s where things get tricky. Not all PPIs are created equal. Omeprazole - the cheapest and most common - interferes with clopidogrel. Clopidogrel needs to be activated by an enzyme in your liver called CYP2C19. Omeprazole blocks that enzyme. Studies show it can reduce clopidogrel’s effectiveness by up to 45%. That means your platelets stay more active. And that raises your risk of another heart attack or stent clot. A 2010 meta-analysis in Circulation found patients on omeprazole and clopidogrel had a 27% higher risk of cardiovascular events. That’s not worth the trade-off. If you’re on clopidogrel, avoid omeprazole. Period.Which PPIs Are Safe with Antiplatelets?
The answer depends on which antiplatelet you’re taking.- If you’re on clopidogrel: Use pantoprazole (40 mg daily) or esomeprazole (20-40 mg daily). Both have minimal effect on CYP2C19. Pantoprazole is the safest bet - it’s been studied the most in this setting.
- If you’re on prasugrel or ticagrelor: You’re fine with any PPI. These drugs don’t rely on CYP2C19. So omeprazole, esomeprazole, or pantoprazole - all are safe. Many doctors default to esomeprazole here because it’s slightly stronger at reducing acid.

PPIs vs. H2 Blockers: Why PPIs Win
You might think famotidine (Pepcid) or ranitidine could work too. They’re cheaper. But they don’t cut it. A 2017 meta-analysis in JAMA Internal Medicine compared PPIs and H2 blockers head-to-head. PPIs reduced upper GI bleeding by 60%. H2 blockers? Only 30%. The difference? 1.8% absolute risk reduction for PPIs versus 0.9% for H2 blockers. That’s not close. If you’re at risk, you need the stronger protection.Who Should Get a PPI? The Real Guidelines
Not everyone needs one. But if you have even one of these risk factors, you should be on a PPI:- Age 65 or older
- History of stomach ulcer or GI bleed
- Taking NSAIDs like ibuprofen or naproxen
- On anticoagulants like warfarin or apixaban
- Using corticosteroids
The Dark Side: When PPIs Do More Harm Than Good
PPIs aren’t harmless. Long-term use - especially without a clear reason - increases risks:- C. difficile infection: Risk goes up by 0.5%. It’s small, but serious - can cause severe diarrhea and hospitalization.
- Community-acquired pneumonia: Risk increases by 0.8%. Less acid means more bacteria survive in the stomach and can travel up.
- Chronic kidney disease: Studies show a 20% higher risk with long-term use.
- Bone fractures: FDA warns about this with high doses over a year.

How Long Should You Take It?
Most guidelines say 6 to 12 months. After that, reassess. If you’re on DAPT for 12 months after a stent, you can often stop the PPI after 12 months too - unless you still have risk factors. But if you’re on extended DAPT - say, 36 months because you had a second heart attack - you likely need the PPI longer. A 2025 study showed PPIs still cut bleeding risk at the 12-month mark, and the benefit continued. Don’t stop it cold turkey. Tapering isn’t usually needed, but if you’ve been on it over a year, talk to your doctor. Stopping suddenly can cause rebound acid, but that’s not dangerous - just uncomfortable.What About Newer Drugs Like Vonoprazan?
There’s exciting news on the horizon. A new drug called vonoprazan - a potassium-competitive acid blocker - is coming to the U.S. in late 2025. It’s stronger than PPIs at blocking acid and doesn’t interfere with clopidogrel at all. In trials, it worked just as well as esomeprazole for stopping GI bleeds - without the drug interaction. It’s not available yet, but if you’re on clopidogrel and need long-term protection, this could be the future. Keep an eye out.What You Can Do Right Now
If you’re on aspirin plus clopidogrel, prasugrel, or ticagrelor:- Ask your doctor: “Am I at risk for GI bleeding?” List any past ulcers, NSAID use, age, or other meds.
- If you’re on clopidogrel, ask: “Is my PPI pantoprazole or esomeprazole?” If it’s omeprazole, ask if you can switch.
- Ask: “Do I really need this long-term?” Don’t assume it’s forever.
- Don’t take OTC PPIs for months without checking in. They’re not meant for long-term use without supervision.
Final Thought: It’s Not About Avoiding Risk - It’s About Managing It
You’re on antiplatelets because the risk of a heart attack or stroke is real. You’re not trying to avoid all side effects - you’re trying to avoid the ones that kill. GI bleeding is one of them. PPIs are the best tool we have to prevent it - if you pick the right one and use it wisely. The goal isn’t to be on more pills. It’s to stay alive and healthy. That means using the right drug, for the right person, for the right time.Can I take omeprazole with clopidogrel?
No. Omeprazole reduces clopidogrel’s effectiveness by blocking the CYP2C19 enzyme your liver needs to activate it. This can increase your risk of another heart attack or stent clot. Use pantoprazole or esomeprazole instead if you’re on clopidogrel.
Do I need a PPI if I’m on ticagrelor or prasugrel?
If you have risk factors for GI bleeding - like age over 65, prior ulcers, or taking NSAIDs - yes. Ticagrelor and prasugrel don’t interact with PPIs, so you can safely use any of them. Esomeprazole or pantoprazole are both good choices.
How long should I take a PPI with antiplatelets?
Most people take it for 6 to 12 months, especially if they’re on dual therapy after a stent. If you’re on extended therapy (like 36 months), you may need the PPI longer. Always reassess after 12 months with your doctor - don’t just keep taking it by default.
Are H2 blockers like famotidine a good alternative to PPIs?
No. H2 blockers reduce stomach acid less effectively than PPIs. Studies show PPIs cut GI bleeding risk by 60%, while H2 blockers only reduce it by 30%. If you’re at risk, PPIs are the only proven option.
Can I stop my PPI if I feel fine?
Don’t stop without talking to your doctor. Even if you feel fine, you’re still at risk for silent bleeding. Stopping too early can leave you unprotected. But if you’ve been on it over a year and have no risk factors, your doctor might suggest stopping after a reassessment.



Joanna Domżalska, January 26, 2026
So we’re just supposed to trust big pharma’s favorite acid blocker now? Next they’ll tell us to take aspirin for longevity. I’ve seen people on PPIs for 10 years and end up with kidney failure. This isn’t medicine-it’s profit-driven band-aids.
Faisal Mohamed, January 28, 2026
Let’s be real 🤔-this is a classic CYP450 pharmacokinetic tango 🎶. Omeprazole = CYP2C19 inhibitor = clopidogrel prodrug activation blocked = platelet reactivity ↑ = CV risk ↑. Pantoprazole? Minimal inhibition. Esomeprazole? Slightly better. But honestly, we need better tools than this 90s-era chemistry. Vonoprazan? Finally. 🚀💊
Josh josh, January 28, 2026
my doc put me on omeprazole after my stent and i felt fine till i got really sick with c diff and now im paranoid about every pill i take. why dont they just tell you the truth instead of giving you a script and saying "youll be fine"
bella nash, January 30, 2026
It is imperative to acknowledge that the pharmacological interactions between proton pump inhibitors and antiplatelet agents constitute a clinically significant phenomenon requiring meticulous patient evaluation and individualized therapeutic decision-making.
SWAPNIL SIDAM, January 30, 2026
I have seen too many elderly people in India on these pills for years. Their stomachs are fine, but their bones break like dry sticks. Doctor just gives PPI like candy. No one checks if they still need it. Please, stop the blind prescribing.
Curtis Younker, January 31, 2026
Hey everyone, I just want to say this post is seriously life-saving info-I had no idea omeprazole could mess with clopidogrel like that! I’m on ticagrelor and my doc gave me esomeprazole and I was like, "cool, whatever"-now I get it. If you’re on dual therapy, don’t sleep on this. Talk to your doc, ask about your PPI, and don’t let them brush you off. Your gut might be quiet but your heart? It’s screaming for protection. You got this 💪❤️
Henry Jenkins, February 2, 2026
This is one of the clearest summaries I’ve seen on this topic. The CYP2C19 interaction is under-discussed in primary care, and the data on pantoprazole being safer than omeprazole with clopidogrel is solid. But I’m curious-what about genetic polymorphisms? If someone is a poor metabolizer of CYP2C19 anyway, does omeprazole still add risk? And what’s the evidence for tapering PPIs after 12 months? Are there studies on rebound hypersecretion versus continued bleeding risk?
Dan Nichols, February 3, 2026
People are still taking PPIs like they’re vitamins. You’re not a 70-year-old on warfarin and NSAIDs? Then you don’t need it. And no, feeling "fine" doesn’t mean you’re safe. Silent bleeds don’t give you a warning label. Also, H2 blockers? They’re not useless-they’re just not good enough. But neither is taking a PPI for 5 years because your doctor forgot to follow up. Wake up.
Renia Pyles, February 3, 2026
Oh wow so now we’re supposed to believe the same doctors who gave us Vioxx and OxyContin are giving us safe advice? PPIs cause dementia, kidney failure, and nutrient malabsorption. And you’re telling me to take one for a year just to avoid a bleed that might not even happen? I’d rather take my chances with a heart attack than end up on dialysis.
Rakesh Kakkad, February 5, 2026
It is of utmost importance to note that the pharmacological profile of vonoprazan, as a potassium-competitive acid blocker, represents a paradigm shift in gastric acid suppression, particularly in the context of dual antiplatelet therapy. Its non-interference with CYP2C19 enzymatic pathways renders it an ideal candidate for future clinical adoption, pending regulatory approval and long-term outcome data.