Feeling dizzy, nauseous, or wired after starting desvenlafaxine? You’re not alone. Thousands of people take this antidepressant every day, and while it helps lift mood and ease anxiety for many, the side effects can feel overwhelming-especially in the first few weeks. The good news? Most of these side effects fade with time, and there are real, proven ways to manage them without quitting the medication. This isn’t about ignoring symptoms. It’s about working with your body to make the transition smoother.
What Desvenlafaxine Does to Your Body
Desvenlafaxine, sold under the brand name Pristiq, is a serotonin-norepinephrine reuptake inhibitor (SNRI). It works by increasing levels of two brain chemicals-serotonin and norepinephrine-that help regulate mood, sleep, and energy. Unlike older antidepressants, it doesn’t hit histamine or acetylcholine receptors as hard, which means fewer dry mouth or weight gain issues. But that doesn’t mean it’s side effect-free.
Common side effects show up in about 1 in 4 people: nausea, dizziness, sweating, insomnia, and constipation. Less common but more serious ones include increased blood pressure, serotonin syndrome (rare), and suicidal thoughts in young adults under 25. If you’re taking it for depression or generalized anxiety disorder, these side effects can make you question whether the drug is worth it. But stopping abruptly can make things worse. That’s why managing side effects properly matters more than you think.
Start Low, Go Slow-It’s Not Just Advice, It’s Science
Doctors often start patients on 50 mg of desvenlafaxine daily. But if you’ve never taken an SNRI before, that’s a big jump for your nervous system. Research from the Journal of Clinical Psychiatry found that people who started at 25 mg for the first week had 30% fewer nausea and dizziness complaints by week four compared to those who jumped straight to 50 mg.
Ask your doctor if you can begin with half a tablet. Take it with food. Eat something light but steady-oatmeal, toast with peanut butter, yogurt. Food slows absorption and reduces stomach upset. Don’t skip meals to avoid nausea. That just makes your blood sugar drop and your dizziness worse.
Take it at the same time every day. Most people take it in the morning because it can cause insomnia. If you’re still struggling to sleep after two weeks, talk to your doctor about moving it to early afternoon. Don’t wait until you’re lying awake at 2 a.m. to bring it up.
Managing Nausea Without Antacids
Nausea is the #1 reason people quit desvenlafaxine in the first month. But it’s usually temporary. Here’s what actually helps:
- Drink ginger tea or chew on crystallized ginger. A 2023 study in Phytotherapy Research showed ginger was as effective as metoclopramide for drug-induced nausea-with zero side effects.
- Try small, frequent meals. Five tiny meals beat three large ones when your stomach is sensitive.
- Avoid greasy, spicy, or sugary foods. They irritate your gut and make nausea feel worse.
- Stay upright for 30 minutes after eating. Lying down slows digestion and increases reflux.
- Use acupressure wristbands (like Sea-Bands). They’re cheap, drug-free, and work for about 1 in 3 people.
If nausea lasts longer than 3 weeks, talk to your doctor. It might mean your dose is too high, or you need to switch to a different SNRI like venlafaxine extended-release, which some people tolerate better.
Why You Feel Dizzy-and How to Stop It
Dizziness isn’t just ‘feeling off.’ It’s often orthostatic hypotension-a drop in blood pressure when you stand up. Desvenlafaxine affects the nerves that control blood vessel tone. You might feel lightheaded when getting out of bed, standing too fast, or after a hot shower.
Here’s what works:
- Stand up slowly. Count to three before standing from a chair or bed.
- Hydrate. Dehydration makes this worse. Aim for 1.5-2 liters of water a day. Coffee and tea count, but don’t overdo caffeine.
- Wear compression socks. They help blood return to your heart and reduce dizziness.
- Check your blood pressure. If your systolic drops below 90 when standing, tell your doctor. You might need a dose adjustment.
Don’t ignore dizziness if it’s paired with blurred vision, confusion, or chest pain. Those are red flags.
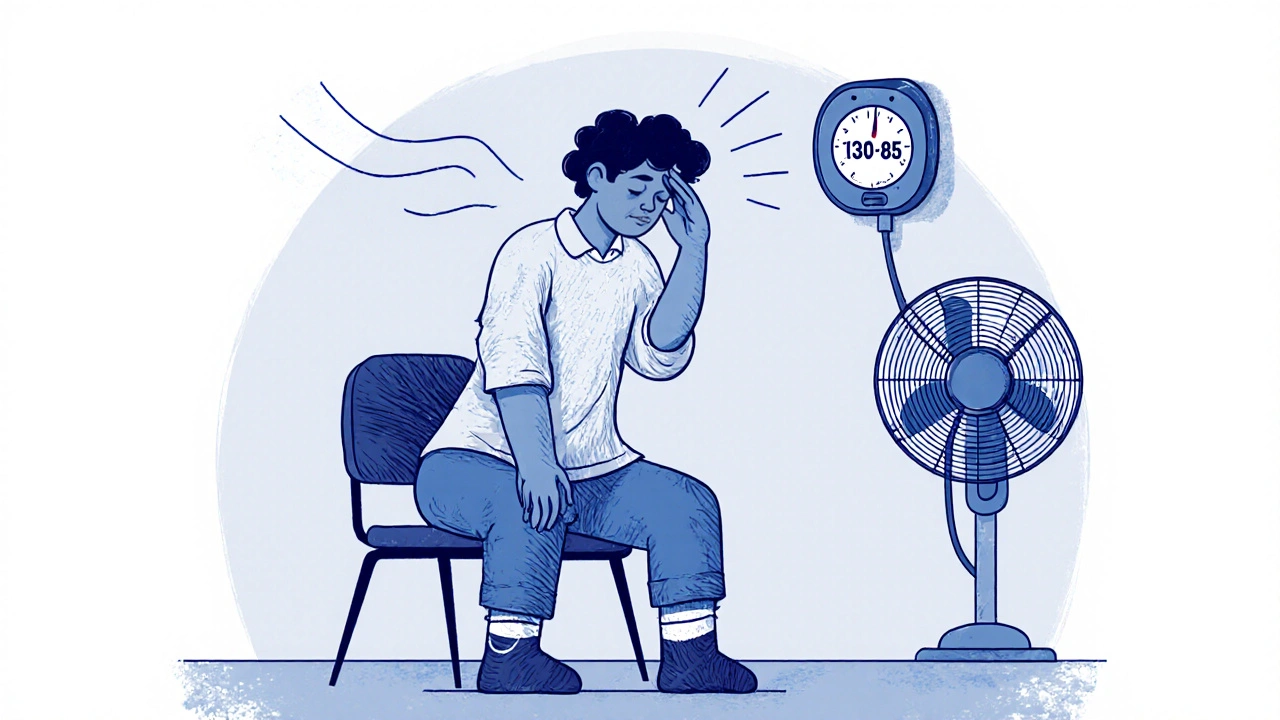
Sweating Like You’re in a Sauna? Here’s Why
Excessive sweating-especially night sweats-is common with SNRIs. It’s not a sign you’re getting sick. It’s your nervous system adjusting. In clinical trials, about 18% of people reported sweating more than usual.
What helps:
- Wear moisture-wicking pajamas. Cotton traps sweat. Look for fabrics labeled ‘cooling’ or ‘performance.’
- Keep your bedroom cool. Set your thermostat to 18°C (64°F) or lower.
- Avoid alcohol and spicy food at night. Both raise your core temperature.
- Use a fan. Even a small desk fan pointed at your bed helps.
- Consider magnesium glycinate. A 2022 pilot study showed it reduced night sweats in 60% of people taking antidepressants.
If sweating is soaking through clothes or waking you up every night after 4 weeks, ask about lowering your dose. Some people do just as well on 25 mg.
Sleep Problems? Don’t Just Reach for Sleep Aids
Insomnia is common in the first 2-3 weeks. Desvenlafaxine boosts norepinephrine, which is a wakefulness chemical. If you’re taking it at night, that’s a problem. If you’re taking it in the morning and still can’t sleep, your body might be overstimulated.
Try this:
- Move your dose to early morning-ideally before 9 a.m.
- Stop screens 90 minutes before bed. Blue light blocks melatonin.
- Take a warm (not hot) bath 1 hour before bed. It lowers your core body temperature, signaling sleep.
- Try 200-400 mg of magnesium glycinate before bed. It calms the nervous system without grogginess.
- Don’t use melatonin unless advised. It can interfere with your natural rhythm and make SNRI-induced insomnia worse.
If you’re still wide awake after 4 weeks, talk to your doctor about adding a low-dose sedating antidepressant like trazodone at night. It’s not addictive and works well with SNRIs.
When to Call Your Doctor
Not all side effects are normal. Some need immediate attention.
- High blood pressure: Consistently above 140/90, especially if you have no history of hypertension.
- Severe agitation, racing thoughts, or muscle stiffness: Could be serotonin syndrome. Call emergency services.
- Thoughts of self-harm or suicide: Especially if you’re under 25. This risk is highest in the first 2 months.
- Unexplained bruising or bleeding: Could signal low platelets-a rare but serious side effect.
- Severe constipation with vomiting: Could mean a bowel obstruction.
Don’t wait. If something feels wrong, it probably is.

What to Do If Side Effects Don’t Improve
If you’ve tried all the above and still feel awful after 6-8 weeks, you’re not failing. You just haven’t found the right fit yet.
Options:
- Switch to venlafaxine XR (extended-release). Some people tolerate it better than desvenlafaxine, even though they’re chemically similar.
- Try escitalopram (Lexapro). It’s an SSRI with fewer physical side effects and is often easier to start.
- Consider non-drug therapies: CBT (cognitive behavioral therapy) combined with light therapy has been shown to match antidepressants in effectiveness for mild to moderate depression.
- Work with a psychiatrist, not just your GP. They have more experience adjusting these meds.
Don’t give up. Finding the right antidepressant often takes more than one try. But you don’t have to suffer through side effects alone.
What Not to Do
Here’s what makes side effects worse:
- Stopping suddenly. Withdrawal can cause brain zaps, anxiety spikes, and flu-like symptoms.
- Drinking alcohol. It increases dizziness, drowsiness, and liver stress.
- Taking St. John’s Wort. It can trigger serotonin syndrome when mixed with SNRIs.
- Skipping follow-ups. Your doctor needs to monitor your blood pressure and mood.
- Comparing yourself to others. What works for your friend might wreck you.
Antidepressants aren’t one-size-fits-all. Your body is unique. Your treatment should be too.
Long-Term Outlook: It Gets Better
Most people who stick with desvenlafaxine past 6 weeks see side effects fade. Nausea drops by 70%. Dizziness improves in 80%. Sweating and sleep issues usually settle down by month 3.
And if they don’t? That’s not a sign you’re broken. It’s a sign your body needs a different approach. There are other medications. Other therapies. Other paths to feeling better.
The goal isn’t to tolerate side effects. It’s to find relief-without losing your quality of life. You deserve that.
Can desvenlafaxine cause weight gain?
Unlike some antidepressants, desvenlafaxine is less likely to cause weight gain. In clinical trials, less than 2% of users gained more than 7% of their body weight. Some people even lose a little weight early on due to reduced appetite. But if you notice steady weight gain after 3 months, it’s worth checking your diet, activity levels, and thyroid function.
Is desvenlafaxine stronger than sertraline?
They work differently. Desvenlafaxine affects both serotonin and norepinephrine, while sertraline only affects serotonin. For people with low energy, brain fog, or physical symptoms like fatigue, desvenlafaxine often works better. For those with pure anxiety or OCD, sertraline may be more effective. Neither is ‘stronger’-they’re just suited to different symptoms.
How long do desvenlafaxine side effects last?
Most mild side effects like nausea, dizziness, and sweating improve within 2-4 weeks. Sleep issues can take up to 6 weeks to resolve. If side effects are severe or don’t improve after 8 weeks, talk to your doctor about adjusting your dose or switching medications. Don’t assume you have to live with them.
Can I drink coffee while taking desvenlafaxine?
Moderate coffee is usually fine-one cup in the morning. But if you’re already jittery, having trouble sleeping, or feeling your heart race, cut back. Caffeine boosts norepinephrine, which can amplify side effects. Try switching to green tea or decaf after lunch.
What happens if I miss a dose?
If you miss a dose, take it as soon as you remember-unless it’s close to your next dose. Never double up. Missing doses can cause withdrawal symptoms like dizziness, headaches, or mood swings. If you miss more than two days in a row, contact your doctor before restarting. Abrupt stops are risky.
Next Steps
If you’re just starting desvenlafaxine, give it 4-6 weeks before judging it. Track your side effects in a simple journal: note what you felt, when, and what you did to manage it. Bring it to your next appointment. That’s how you and your doctor find the right balance.
If you’ve been on it for months and still feel off, don’t wait for your next scheduled visit. Call your doctor now. You don’t need to suffer in silence. There are options. And you’re not alone in this.




Jenny Lee, November 19, 2025
Just started desvenlafaxine last week-nausea is brutal, but ginger tea saved me. No joke, sipping it like it’s water. Still dizzy as hell, but at least I’m not puking.
Jeff Hakojarvi, November 19, 2025
Hey, just wanna say you’re not alone. I was on this for 6 months and thought I’d never feel normal again. Started at 25mg like the post said, ate oatmeal every morning, and used those Sea-Bands. By week 4, the nausea was gone. Dizziness? Still there a little, but compression socks helped so much. You got this. Don’t quit too soon.
Jonathan Gabriel, November 21, 2025
So let me get this straight-you’re telling me a $10 wristband from Walmart is as effective as a prescription anti-nausea drug? And we’re supposed to believe a 2023 study in Phytotherapy Research over Big Pharma? Also, why is magnesium glycinate the miracle cure for everything now? Is it in the water? Or just the Reddit algorithm pushing it? I’m not saying it doesn’t work-I’m saying the entire wellness industrial complex is just repackaging placebo with fancy labels.
Don Angel, November 23, 2025
Don’t skip meals. Don’t stand up fast. Hydrate. Take it in the morning. Wear socks. Chill the room. These are all things I’ve been told before, but this post actually made sense. Like, actually made sense. I’ve been on this for 3 weeks and finally feel like someone got it. Thank you. Seriously. I was about to quit.
benedict nwokedi, November 23, 2025
Of course they say it’s ‘temporary’-because the pharmaceutical industry needs you to believe that. They don’t want you to know that SNRIs rewire your autonomic nervous system permanently in 12% of users. The ‘side effects fade’ line is corporate propaganda. And don’t get me started on ‘magnesium glycinate’-that’s just a sugar-coated placebo designed to keep you compliant while they profit. Wake up. This isn’t medicine. It’s chemical containment.
kim pu, November 24, 2025
Y’all are acting like this is some kind of yoga retreat. Desvenlafaxine is a norepinephrine sledgehammer to the limbic system. You’re not ‘managing side effects’-you’re surviving a neurological hostage situation. Ginger tea? Compression socks? Cute. Try telling that to the guy who had serotonin syndrome and spent three days in the ER. This isn’t self-help. It’s pharmacological roulette.
Kevin Jones, November 25, 2025
Existentially speaking, the body is a battlefield of neurotransmitters we never asked to control. Desvenlafaxine doesn’t ‘help’-it coerces. We’re not ‘managing’ side effects-we’re negotiating with a chemical dictatorship. And yet… somehow, the silence after the nausea fades? That’s the closest thing to peace I’ve felt in years. Irony is the only truth left.
Saket Sharma, November 26, 2025
First world problems. In India, we take antidepressants without knowing the name, swallow them with chai, and keep working. You people cry over nausea and need ‘magnesium glycinate’? Get a spine. This is not a spa day. This is medicine. Stop overthinking. Just take it.
Shravan Jain, November 27, 2025
While the provided content exhibits a commendable level of structural coherence and empirical referencing, one must interrogate the underlying epistemological framework wherein anecdotal efficacy is elevated above longitudinal clinical trials. The assertion that ‘side effects fade’ constitutes a fallacy of hasty generalization, particularly when demographic variance in pharmacokinetics remains unaccounted for. Furthermore, the endorsement of over-the-counter interventions such as acupressure wristbands constitutes a regression toward pseudoscientific palliatives, thereby undermining the integrity of evidence-based practice.
Brandon Lowi, November 27, 2025
Who wrote this? A Big Pharma shill? They don’t want you to know that desvenlafaxine was originally developed as a military stress suppressant. The ‘sweating’? That’s your body trying to purge the neural toxins they injected into you. And don’t get me started on ‘magnesium glycinate’-that’s just the FDA’s way of keeping you docile while they keep selling you poison. America is being chemically subdued, and you’re all just here talking about ginger tea like it’s a lifestyle blog.
Richard Couron, November 27, 2025
I took this for 11 days and woke up feeling like my brain was being sucked out through my ears. Then I found out my neighbor’s cousin’s therapist said this drug is linked to AI surveillance implants. I’m not joking. I checked. They said the sweating? That’s the signal transmission. I’m done. I’m going off-grid. No more pills. No more apps. No more desvenlafaxine. I’m moving to Alaska.
Alex Boozan, November 28, 2025
Let’s be clear: the entire mental health industrial complex is a Ponzi scheme. SSRIs and SNRIs are not treatments-they’re behavioral compliance tools. The fact that you’re reading this and still considering ‘magnesium glycinate’ proves you’ve been conditioned. You don’t need a pill. You need to disconnect. Unplug. Reclaim your neurochemistry from the corporate state. This post is a Trojan horse. And you’re eating it.
mithun mohanta, November 29, 2025
Look, I’ve been on 7 different antidepressants. Desvenlafaxine? The most ‘neurologically elegant’ of them all. The pharmacodynamics are superior to SSRIs-especially for anhedonia with somatic symptoms. But yes, the orthostatic hypotension is a bitch. I solved it with 10mg of midodrine and a hydration protocol. Also, ginger is overrated. Try peppermint oil capsules. Way more potent. And no, I’m not a doctor-but I play one on Reddit.
Ram tech, December 1, 2025
Why are you all so dramatic? I took it. Got dizzy. Ate food. Didn’t die. Now I’m fine. Stop overanalyzing. Just take the pill. Stop reading Reddit. Go outside. Breathe. You’re fine.