PML Risk Calculator
This tool helps you understand your risk of Progressive Multifocal Leukoencephalopathy (PML) based on the immunosuppressant therapy you're receiving and your individual risk factors. Note: This calculator is for educational purposes only and should not replace professional medical advice.
Enter Your Information
What is Progressive Multifocal Leukoencephalopathy (PML)?
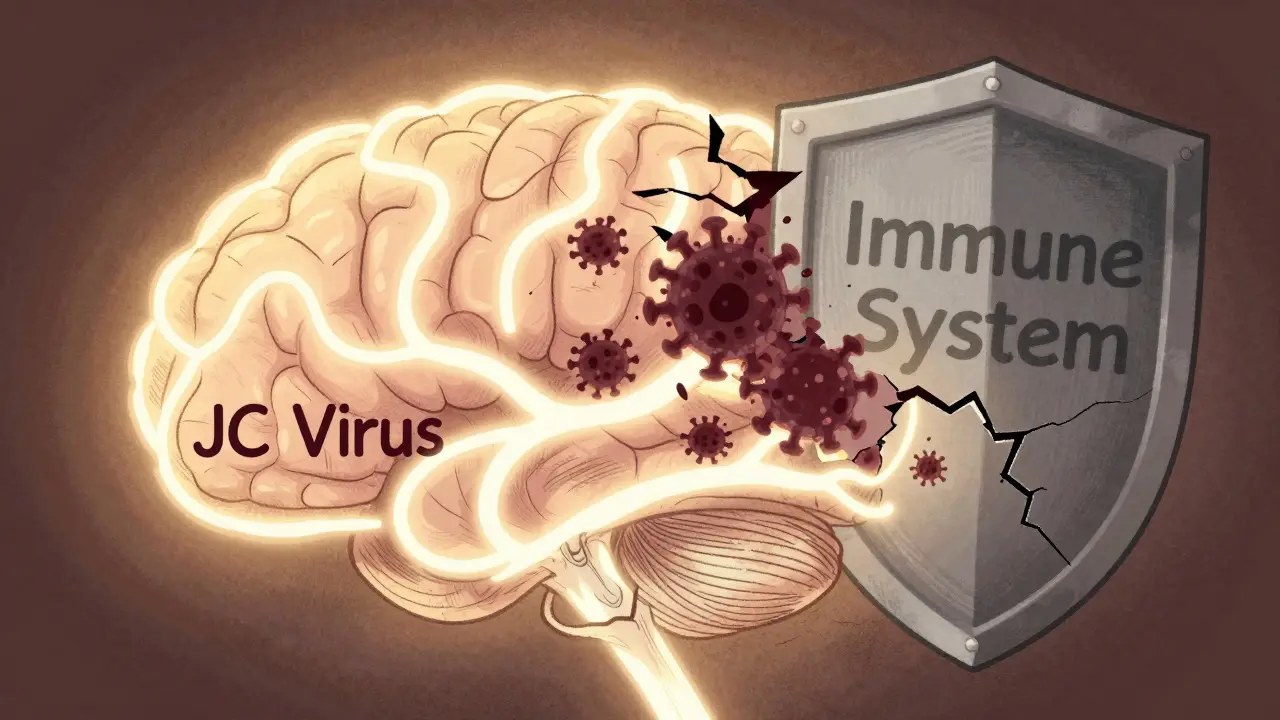
PML is a rare but deadly brain disease caused by the John Cunningham (JC) virus. Most people carry this virus without knowing it-between 50% and 70% of adults have been exposed. It stays quiet in the kidneys and bone marrow, harmless as long as your immune system is strong. But when you take certain immunosuppressant drugs, your body loses the ability to keep the virus in check. That’s when it wakes up, attacks the white matter of your brain, and destroys the protective coating around nerve cells. The result? Progressive neurological damage that can lead to paralysis, vision loss, speech problems, and even death.
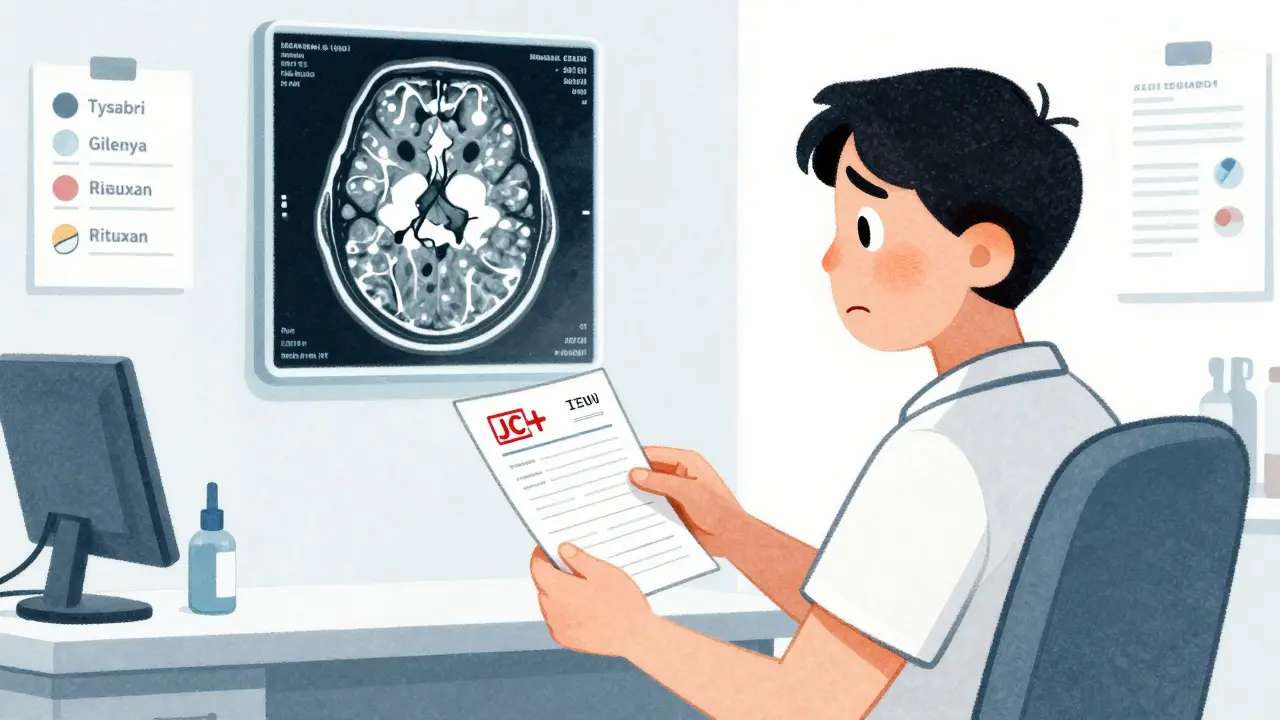
Which immunosuppressants carry the highest PML risk?
Not all immunosuppressants are created equal when it comes to PML risk. The biggest red flag is natalizumab (Tysabri), a drug used for multiple sclerosis and Crohn’s disease. Through 2011, 102 confirmed PML cases were reported among 82,732 patients on natalizumab worldwide. That’s about 0.12% overall-but the risk skyrockets if you have three things: a positive JC virus antibody test, prior use of another immunosuppressant like azathioprine or methotrexate, and treatment lasting longer than two years. In that high-risk group, PML hits at a rate of 4.1 cases per 1,000 patients.
Other drugs with notable PML risk include fingolimod (Gilenya) (0.4 cases per 1,000 patient-years), dimethyl fumarate (Tecfidera) (0.2 cases per 1,000), and rituximab (Rituxan) (0.8 cases per 1,000). For blood cancer patients, ibrutinib (Imbruvica) has shown a 0.3% PML incidence in clinical trials. Meanwhile, older MS drugs like interferon beta and glatiramer acetate have never been linked to a single confirmed case of PML.
How is PML risk measured-and why it’s not simple
The main tool doctors use to predict PML risk is the JC virus antibody test. It tells you if you’ve ever been exposed to the virus. But here’s the catch: 2-3% of people who test negative still carry the virus. These false negatives are real, and they’ve caught even experienced neurologists off guard. One Reddit user described how their neurologist missed early PML lesions on MRI because their JC antibody test came back negative-only to find lesions later.
There’s also the JC virus antibody index, a more detailed measure that shows how strong your immune response to the virus is. People with an index above 1.5 have a 10.9% cumulative risk of PML after four years on natalizumab. Those below 0.9? Just 0.09%. This number helps doctors decide whether to keep you on the drug or switch you out.
But even these tools aren’t perfect. The American Academy of Neurology warns that patients with low lymphocyte counts (below 0.8 x 10⁹/L) are at 4.3 times higher risk-and current risk models don’t fully account for this. That means someone could have a low antibody index but still be in danger because their immune system is too weak overall.
What does PML feel like? Recognizing the early signs
PML doesn’t hit with a bang. It creeps in. Symptoms are often mistaken for a flare-up of multiple sclerosis or another underlying condition. That’s why so many cases-37% according to one study-are misdiagnosed at first.
Early signs include:
- Mild trouble speaking or slurred speech
- Blurred or lost vision in one eye
- Weakness on one side of the body
- Loss of coordination or clumsiness
- Changes in thinking or memory
- Unexplained fatigue that doesn’t improve with rest
These symptoms don’t come and go like an MS relapse. They get worse over weeks, not days. If you’re on a high-risk drug and notice even one of these changes, don’t wait. Tell your neurologist immediately. Early detection saves function-and lives.
How doctors monitor for PML
There’s no cure for PML once it takes hold. The only way to stop it is to catch it early-and that means regular monitoring. The Cleveland Clinic recommends brain MRIs every 3 to 6 months for patients on natalizumab or other high-risk drugs. These scans look for abnormal bright spots in the white matter of the brain, especially using diffusion-weighted imaging, which picks up early changes invisible on standard scans.
But reading these MRIs isn’t easy. Neurologists and radiologists need 15-20 hours of special training to tell the difference between PML lesions and regular MS plaques. That’s why many community clinics struggle to catch PML early. Academic medical centers have standardized protocols in place-92% of them do. Only 67% of private practices do.
On top of imaging, the FDA requires doctors to check your JC virus antibody status before starting natalizumab. They also ask: “Have you ever taken another immunosuppressant?” If the answer is yes, your risk jumps 3-6 times higher. That’s why many patients who previously took drugs like methotrexate or azathioprine are switched to safer alternatives.
What happens after PML is diagnosed?
Stopping the immunosuppressant is step one. But that’s not enough. In 50-60% of cases, the immune system comes back too hard. This is called immune reconstitution inflammatory syndrome (IRIS). Your body, now trying to fight the virus, ends up attacking your brain tissue instead. That can cause swelling, seizures, and even death.
Managing IRIS requires steroids like methylprednisolone to calm the immune response. One patient on Reddit shared that after stopping natalizumab and starting steroids, he regained 90% of his motor function over six months. That’s rare-but it happens. Survival rates are still grim: 30-50% of PML patients die. Of those who live, most have lasting neurological damage.

What’s new in PML treatment and prevention?
The good news? Research is moving fast. In 2024, a pilot study of DIAVIS T-cell therapy showed a 68% reduction in death and 45% improvement in function among 17 PML patients. That’s not a cure yet, but it’s the first real sign of progress.
Another promising angle: maraviroc, a drug originally used for HIV. The Cleveland Clinic is now testing it in a Phase II trial (NCT05678901) to see if it can block the JC virus from entering brain cells. Early lab results suggest it might prevent PML in high-risk patients on natalizumab.
Immune checkpoint inhibitors like pembrolizumab and nivolumab are also being tried in small numbers of patients. In 27% of cases, they helped the immune system regain control without triggering dangerous IRIS. These aren’t standard yet-but they’re giving hope.
How patients are responding to PML risk
On MS forums, anxiety about PML is overwhelming. In one survey of 214 patients, 78% said they felt extreme fear about developing PML. Over half said they’d stop natalizumab after two years-even if it was controlling their MS perfectly.
That fear is driving real behavior changes. Since 2015, prescriptions for natalizumab have dropped 22% in patients with prior immunosuppressant use. Meanwhile, drugs like ocrelizumab have seen a 35% rise in use in this group. Patients aren’t just trusting their doctors-they’re doing their own research, asking hard questions, and switching therapies to reduce risk.
It’s not just about survival. It’s about quality of life. One patient wrote: “I’d rather have a little more MS than risk losing my ability to walk, talk, or recognize my own kids.” That sentiment is shared by thousands.
What should you do if you’re on an immunosuppressant?
- Know your JC virus status. Get tested before starting any high-risk drug. Retest every 6 months if you’re on natalizumab.
- Tell your doctor about every past immunosuppressant. Even if it was years ago. Azathioprine, methotrexate, cyclophosphamide-they all add up.
- Get regular MRIs. Don’t wait for symptoms. Early lesions are treatable. Late ones are not.
- Track your symptoms. Write down any new weakness, vision changes, or speech issues. Don’t assume it’s your MS.
- Ask about alternatives. If your risk is high, is there a safer drug that works just as well?
The goal isn’t to scare you. It’s to empower you. PML is rare-but it’s real. And with the right monitoring, you can keep your disease under control without putting your brain at risk.



Danielle Stewart, December 17, 2025
Just wanted to say this post saved my life. I was on Tysabri for 22 months, had a negative JC test, and started having slurred speech. My neurologist brushed it off as ‘MS fatigue.’ I pushed for an MRI - turns out, early PML lesions. Caught it because I read this. Don’t ignore tiny changes. You know your body best.
Sajith Shams, December 18, 2025
Everyone’s panicking over 0.12% risk like it’s a pandemic. Let’s be real - you’re more likely to die from a car crash on the way to your infusion center. The real problem? Pharma companies hiding data and doctors not being trained to read MRIs properly. Stop blaming the drug - blame the system that lets untrained radiologists interpret scans.
Glen Arreglo, December 18, 2025
As someone who moved from the US to India and switched from natalizumab to ocrelizumab, I can tell you the access gap is real. Back home, I got MRIs every 3 months and a JC index test every 6. Here? I waited 9 months for a scan. No one even asked about my past methotrexate use. This isn’t just medical - it’s a global equity issue.
shivam seo, December 20, 2025
Another anti-pharma scare piece. People on immunosuppressants are literally choosing to be sick because they’re too lazy to exercise or eat right. PML? Rare. But so is getting struck by lightning. Stop making people feel guilty for taking medicine that lets them live. If you want to be healthy, stop being a medical drama queen.
benchidelle rivera, December 22, 2025
It’s imperative to emphasize that the JC virus antibody index is not a diagnostic tool - it’s a risk stratification metric. The American Academy of Neurology guidelines explicitly state that patients with lymphocyte counts below 0.8 x 10⁹/L require heightened surveillance regardless of antibody status. This is not optional. This is standard of care. If your provider isn’t discussing lymphocyte counts, seek a second opinion immediately.
Matt Davies, December 22, 2025
Reading this felt like someone handed me a flashlight in a cave I didn’t even know I was lost in. I thought my ‘brain fog’ was just stress. Turns out, it was PML whispering in my ear. Now I’m off natalizumab, doing weekly MRIs, and honestly? I’d rather have a few more MS flares than lose my ability to hold my daughter’s hand. This isn’t fear-mongering - it’s survival wisdom wrapped in data.
Ashley Bliss, December 23, 2025
They say knowledge is power - but what if the knowledge is weaponized? Who gets to decide who lives and who dies when the cost of treatment is your brain? We’re not patients. We’re statistical outliers in a corporate algorithm. The JC virus doesn’t care about your insurance. The drug companies don’t care about your children. And your neurologist? They’re just following a checklist written by a board that’s never held a dying patient’s hand. We’re not just risking PML - we’re risking our humanity.
Dev Sawner, December 25, 2025
It is a well-documented fact that the incidence of PML in patients with prior exposure to immunosuppressants such as azathioprine is statistically significant (p < 0.001) when combined with prolonged natalizumab therapy. Furthermore, the sensitivity of the JC virus antibody assay is approximately 97–98%, meaning that false negatives are not merely theoretical - they are clinically consequential. Therefore, it is imperative that clinicians integrate lymphocyte count monitoring as a mandatory adjunctive parameter, as per the 2023 AAN practice advisory update.
Moses Odumbe, December 25, 2025
Bro, I was on Tecfidera for 18 months. Got a positive JC test. Switched to Ocrevus. No more panic. But here’s the wild part - my doc didn’t even mention the antibody index until I asked. Now I check my numbers every 6 months like it’s my Netflix subscription. 📊🧠 Don’t wait for symptoms. Know your stats. Stay sharp.
Meenakshi Jaiswal, December 27, 2025
I’m a nurse in Mumbai who works with MS patients. I’ve seen too many people stop their meds because they’re scared of PML - and then end up in the hospital from uncontrolled relapses. The key isn’t to avoid all risk - it’s to manage it. Get tested. Track your counts. Ask about MRI protocols. You don’t need to be a doctor to be your own advocate. Small steps save lives.
bhushan telavane, December 28, 2025
My cousin in Delhi got PML on rituximab for lupus. He was 34. No prior immunosuppressants. Negative JC test. They missed it for 4 months. Now he’s in a wheelchair. This isn’t just an American problem. We need better awareness here - doctors still think MS is ‘a rich person’s disease.’
Mahammad Muradov, December 30, 2025
It is illogical to suggest that patients should switch therapies based on fear alone. The probability of developing PML remains lower than the risk of fatal complications from uncontrolled multiple sclerosis. To abandon effective treatment due to media-driven anxiety is not prudent - it is medically irresponsible. The burden of disease progression far outweighs the statistical likelihood of PML in the absence of multiple risk factors.
Connie Zehner, December 30, 2025
OMG I’m so glad I found this. I’ve been on Tysabri for 3 years, positive JC, index 1.7… and I’ve been having weird tingling in my left hand. I thought it was just stress. But now I’m crying. I’m so scared. I need to know - am I going to die? Should I tell my husband? I can’t sleep. I’m googling PML symptoms at 3am. Someone please tell me I’m not alone. 😭