GI Bleeding Risk Calculator
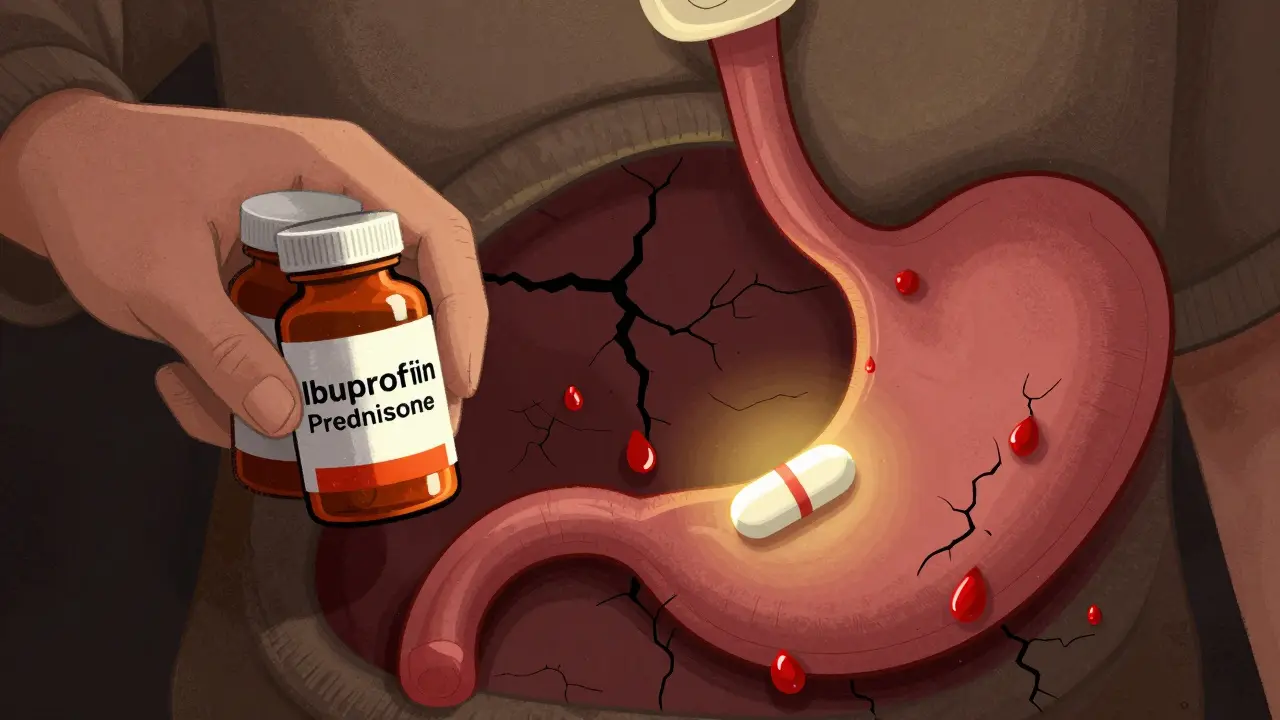
Take a common scenario: someone with arthritis is on daily ibuprofen for pain. Then they get a bad flare-up and their doctor prescribes a short burst of prednisone to calm things down. It seems harmless - two widely used drugs. But together, they create a silent danger that can lead to life-threatening bleeding in the stomach or intestines. This isn’t rare. It’s happening every day in clinics and homes across the country, often without warning.
Why This Combination Is So Dangerous
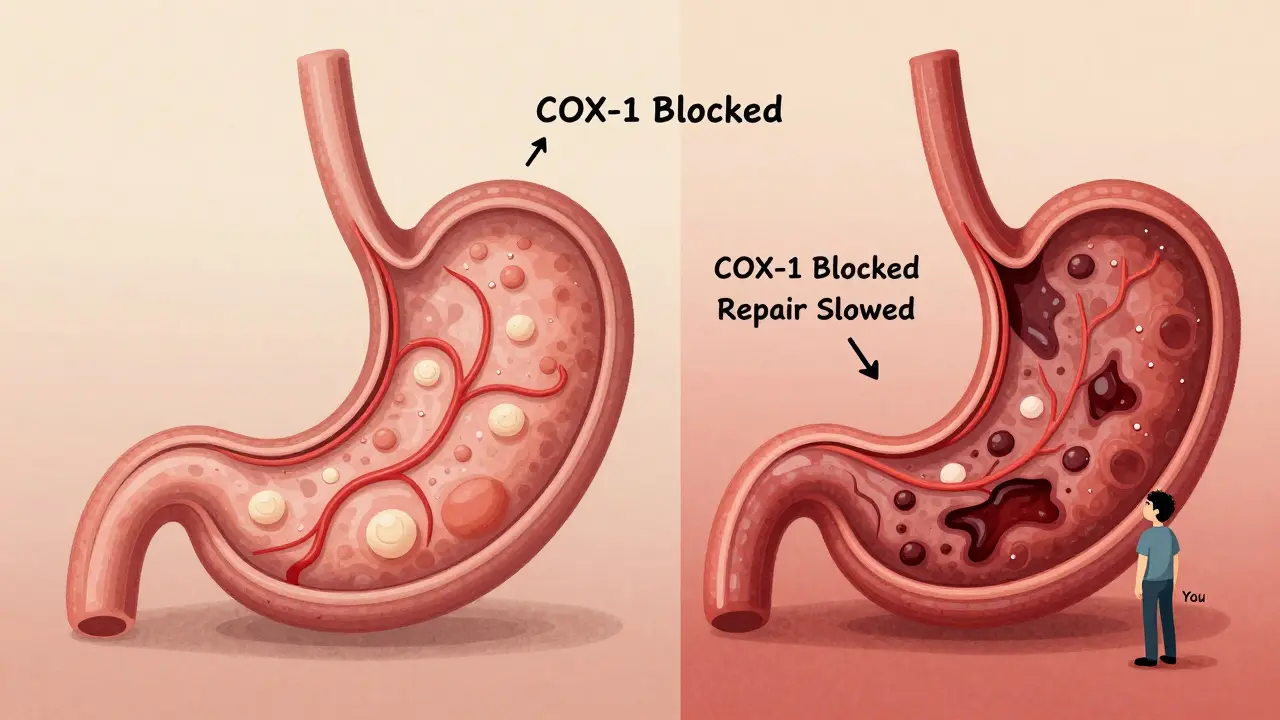
NSAIDs like ibuprofen, naproxen, and diclofenac work by blocking enzymes that cause pain and swelling. But they also block another enzyme - COX-1 - that protects the lining of your stomach. Without it, your stomach loses its natural defense: less mucus, less blood flow, and slower healing. That’s why even a single NSAID can cause ulcers and bleeding in some people. Now add steroids - like prednisone or methylprednisolone. These drugs don’t directly damage the gut. Instead, they make the damage from NSAIDs worse. Steroids slow down tissue repair, reduce mucus production, and mask symptoms. You might feel less pain, but that doesn’t mean your stomach is healing. It means you’re not noticing the bleeding until it’s severe. The numbers don’t lie. If you take an NSAID alone, your risk of upper GI bleeding goes up about four times. If you take a steroid alone, it’s about 1.8 times higher. But when you take both? The risk jumps to nearly 9 times higher than someone taking neither. For people on high-dose NSAIDs - say, more than 1200mg of ibuprofen daily - the risk skyrockets to over 12 times. And it’s not just upper GI. About one-third of NSAID-related bleeds happen in the lower intestine. These are harder to detect, often showing up as sudden anemia or dark stools. Many patients don’t realize what’s happening until they’re in the ER.Who’s at the Highest Risk?
Not everyone who takes steroids and NSAIDs will bleed. But some people are sitting on a ticking clock. These are the red flags:- Age 65 or older
- History of peptic ulcer or GI bleeding
- Taking blood thinners like warfarin or apixaban
- Using multiple NSAIDs at once (e.g., ibuprofen + aspirin)
- High-dose NSAIDs (diclofenac ≥100mg/day, ibuprofen ≥1200mg/day)
- Long-term steroid use - even short bursts of 5-7 days can trigger risk

What Doctors Should Be Doing - But Often Aren’t
The American College of Gastroenterology, the European Society of Gastrointestinal Endoscopy, and the American Gastroenterological Association all agree: if you’re on both steroids and NSAIDs, you need a proton pump inhibitor (PPI) - not just a suggestion, but a standard of care. PPIs like omeprazole, esomeprazole, or pantoprazole reduce stomach acid enough to let the lining heal. They’re not perfect, but they cut the risk of ulcers by more than half compared to no protection. H2 blockers like famotidine? They’re not enough. Studies show they’re 48% less effective than PPIs at preventing NSAID-induced ulcers. Here’s the problem: only about 39% of patients on this combo actually get a PPI prescribed. In non-specialist clinics - think primary care or urgent care - the rate drops to 22%. Why? Because many providers don’t know the data. Or they assume the steroid burst is too short to matter. Or they think the patient will just stop the NSAID soon. But here’s the truth: risk spikes within 7 days. A 5-day prednisone course can be enough. And many people are already taking OTC NSAIDs - they don’t even tell their doctor. A Reddit post from a gastroenterologist says it best: “I see preventable bleeds weekly from primary care providers starting prednisone bursts in patients already on chronic ibuprofen without adding PPIs.”What You Can Do - Even If You’re Not a Doctor
You don’t need to be a medical expert to protect yourself. Here’s what to ask for:- If you’re prescribed a steroid (even a 5-day course), ask: “Am I on an NSAID? Do I need a PPI?”
- If you’re taking OTC ibuprofen or naproxen daily, tell your doctor. Don’t assume it’s “just a painkiller.”
- Ask if a COX-2 inhibitor like celecoxib is an option. These have about half the GI risk of traditional NSAIDs - even when combined with steroids.
- Check if your pharmacy offers combo pills like Vimovo (naproxen + esomeprazole). These are designed for high-risk patients.
- Watch for warning signs: black or tarry stools, vomiting blood, sudden dizziness, or unexplained fatigue. These aren’t normal. Go to urgent care.
What’s Changing - And What’s Still Missing
Good news: the tide is turning. The FDA now requires boxed warnings on all NSAID labels about GI bleeding. The EMA added specific language about steroid interactions in 2019. New drugs like Vimovo are gaining traction. And systems like Kaiser Permanente and Mayo Clinic have cut bleeding events by nearly 70% by automatically prescribing PPIs when both drugs are ordered together. But here’s the gap: most community pharmacies and small clinics still don’t have clinical decision support built into their systems. If your doctor types “ibuprofen” and “prednisone,” nothing pops up saying, “Warning: High risk of GI bleed. Consider PPI.” Also, many patients still think “steroids are just for inflammation” and don’t realize how deeply they interfere with healing. A 2023 survey found 63% of patients who suffered a GI bleed from this combo had never been warned about the risk.The Bottom Line
Steroids and NSAIDs aren’t evil drugs. They help millions. But together, they’re a dangerous pair - one that’s been known for over 20 years. The science is clear. The guidelines are solid. The tools to prevent bleeding exist. What’s missing is awareness. And action. If you’re on either of these drugs - especially both - don’t wait for symptoms. Talk to your doctor. Ask for a PPI. Ask if there’s a safer alternative. Ask if your risk has been assessed. Because the next time you feel pain, you shouldn’t be risking your life just to relieve it.Can I take ibuprofen with prednisone if I only use it occasionally?
Even occasional use can be risky. Studies show the risk of GI bleeding rises within 7 days of starting both drugs together. If you take ibuprofen even once a week and get a short prednisone course, your risk still increases significantly. It’s not about frequency - it’s about the combination. If you need pain relief while on steroids, ask your doctor about acetaminophen (Tylenol) instead, which doesn’t carry the same GI risk.
Is a PPI safe to take long-term?
PPIs are generally safe for short-term use, which is what’s needed when taking steroids and NSAIDs together. For most people, taking a PPI for a few weeks or months carries minimal risk. Long-term use (over a year) may slightly increase the risk of bone fractures, low magnesium, or certain infections - but these risks are far lower than the danger of a GI bleed. If you’re on this combo for more than a few months, your doctor should reassess whether you still need both drugs and whether you still need the PPI.
Are there NSAIDs that are safer with steroids?
Yes. COX-2 inhibitors like celecoxib have about 50-60% lower risk of GI bleeding than traditional NSAIDs like naproxen or ibuprofen. While they still carry some risk when combined with steroids, the increase is much smaller. For patients over 65 or with prior ulcers, guidelines now recommend COX-2 inhibitors over traditional NSAIDs when steroids are needed. However, celecoxib isn’t right for everyone - especially those with heart disease - so always discuss options with your doctor.
I’m on a steroid burst for a cold - do I need to stop my ibuprofen?
Yes. Steroid bursts for viral illnesses (like colds or flu) are often unnecessary and overused. But if you’re prescribed one, you should avoid NSAIDs entirely during that time. Use acetaminophen for fever or pain instead. Many people don’t realize that OTC NSAIDs are just as risky as prescription ones when combined with steroids. Your body doesn’t care if the drug was bought at a pharmacy or given by a doctor - the interaction is the same.
What if I can’t afford a PPI?
Many PPIs are available as low-cost generics. Omeprazole 20mg can cost less than $5 for a 30-day supply at most U.S. pharmacies. If you’re in the UK or another country with public healthcare, ask your pharmacist - PPIs are often available over the counter or at low cost. Don’t skip protection because of cost. A single GI bleed can cost tens of thousands in hospital care. Prevention is cheap. Bleeding is not.
Can I use natural remedies like turmeric or ginger instead of NSAIDs?
Turmeric and ginger have mild anti-inflammatory effects, but they’re not strong enough to replace NSAIDs for moderate to severe pain. There’s no reliable evidence they prevent GI damage from NSAIDs or steroids. Relying on them as a substitute can be dangerous if you’re still taking NSAIDs. If you want to reduce NSAID use, talk to your doctor about physical therapy, heat therapy, or other non-drug options - not unproven supplements.



Solomon Ahonsi, February 3, 2026
This is why medicine is a joke. Doctors hand out prednisone like candy and never mention the GI bomb they’re handing you with it. I got a 5-day course last year for a sinus thing, was already on ibuprofen for my back, and woke up in the ER with a bleed. No one warned me. Not my PCP, not the urgent care doc, not even the pharmacist. Just ‘take this, feel better.’ Yeah, I felt better-until I almost died. Stop pretending this is ‘common sense.’ It’s negligence.
George Firican, February 4, 2026
The tragedy here isn’t just the combination-it’s the systemic failure to treat pharmacology as a dynamic system rather than a checklist of isolated prescriptions. We’ve reduced human physiology to a series of drug-target interactions, ignoring the cascading biological consequences. The stomach isn’t just a passive tube; it’s a living, healing ecosystem. NSAIDs cripple its defenses. Steroids suppress its repair mechanisms. Together, they’re like turning off the fire alarm while pouring gasoline on the floor. And yet, we act surprised when the building burns down. The solution isn’t just PPIs-it’s a cultural shift in how we think about prescribing. Every drug has a story. We need to read the whole damn book.
Matt W, February 5, 2026
I’m so glad someone finally put this out there. My mom had a GI bleed last winter after a steroid shot and her daily Advil. She didn’t even know they could do that. I spent weeks in the hospital with her, watching her lose blood and strength while the docs just shrugged. The fact that only 39% of patients get a PPI? That’s not just a gap-it’s a massacre. I wish I’d known this before. Now I tell everyone: if you’re on steroids, ask for the PPI. Don’t wait until you’re vomiting black stuff.
Anthony Massirman, February 6, 2026
Just stop taking ibuprofen with steroids. Use Tylenol. Done.
Eli Kiseop, February 8, 2026
i never knew steroids made NSAIDs worse like that i thought they just helped with inflammation why do they mess with healing is it because they suppress the immune system or something
Ellie Norris, February 10, 2026
Oh my gosh this is so important! I’ve seen so many patients on both and no one ever mentions PPIs. I’m a nurse and I’ve had to gently remind doctors more times than I can count. And the cost thing? So many people think PPIs are expensive but omeprazole is like $3 at Walmart. Please don’t skip it. Your gut will thank you. And yes, even a 5-day steroid course counts. Seriously.
Marc Durocher, February 11, 2026
Let me get this straight-doctors are prescribing two drugs that together increase bleeding risk by 900%, and the solution is to slap on a $5 pill that reduces that risk by 50%... but they don’t? And we’re surprised people end up in the ER? This isn’t medicine. This is a comedy of errors written by someone who’s never read a textbook. I’ve got a cousin who almost died from this exact combo. No warning. No PPI. Just ‘you’ll be fine.’
larry keenan, February 12, 2026
The pharmacokinetic and pharmacodynamic interactions between nonsteroidal anti-inflammatory agents and glucocorticoids are well-documented in the literature, particularly in relation to prostaglandin synthesis inhibition and mucosal cytoprotection. The relative risk elevation for upper gastrointestinal hemorrhage is statistically significant (p < 0.001) when both classes are co-administered, with a number needed to harm (NNH) of approximately 12.5 over a 30-day exposure window. Proton pump inhibitors demonstrate a relative risk reduction of 52–68% in this context, per meta-analyses from the Cochrane Collaboration. Clinical decision support systems remain underutilized in ambulatory settings, contributing to persistent underprescribing of gastroprotection.
Nick Flake, February 13, 2026
THIS IS WHY WE NEED TO STOP TREATING DRUGS LIKE LEGO BRICKS 🚨 We stack them like ‘oh this one for pain, this one for swelling’ and forget we’re building a house on quicksand. 💔 I’ve seen people cry in the ER because they didn’t know ibuprofen + prednisone = internal bleeding party. 🤕 PPIs aren’t a ‘bonus’-they’re a seatbelt. And if your doctor doesn’t hand you one? Ask for it. Demand it. Or switch docs. Your stomach isn’t a suggestion box. 🙏 #PPIsSaveLives