When your kidneys aren't working well, what you eat isn't just about taste or comfort-it can mean the difference between staying out of the hospital and facing life-threatening complications. A renal diet isn’t a fad or a quick fix. It’s a medically backed way to take some of the burden off your kidneys and keep dangerous minerals from building up in your blood. For people with stage 3 to 5 chronic kidney disease (CKD), this isn’t optional. It’s essential.
Why Sodium, Potassium, and Phosphorus Matter
Your kidneys filter waste, balance fluids, and regulate minerals like sodium, potassium, and phosphorus. When they’re damaged, they can’t do this job well. Too much sodium makes your body hold onto water, raising blood pressure and swelling your ankles or lungs. High potassium can mess with your heart rhythm-levels above 5.5 mEq/L can trigger dangerous arrhythmias or even cardiac arrest. Phosphorus, when it builds up, pulls calcium out of your bones and deposits it in your blood vessels, heart, and skin, leading to fractures, heart disease, and severe itching.
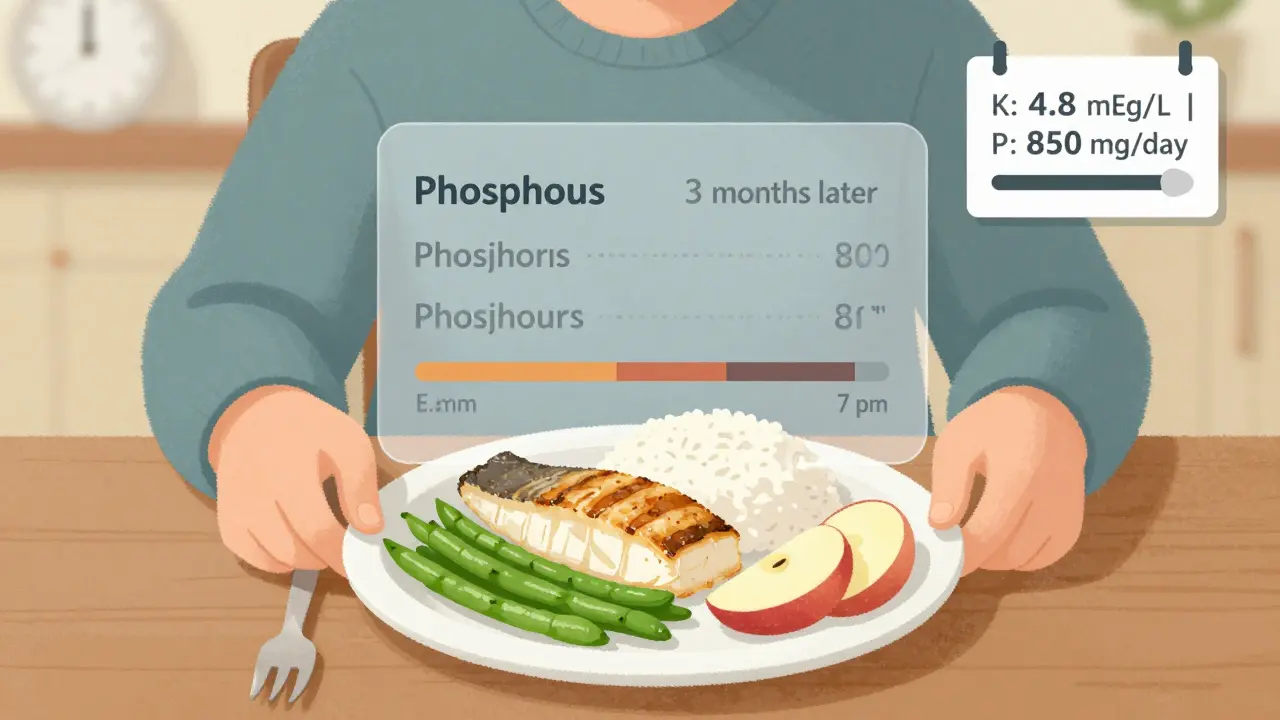
The numbers matter. For non-dialysis CKD patients, the KDIGO 2023 guidelines recommend no more than 2,000-2,300 mg of sodium per day. That’s about one teaspoon of salt. For potassium, most experts suggest 2,000-3,000 mg daily, but your doctor may adjust that based on your blood tests. Phosphorus should stay under 800-1,000 mg per day. Sounds simple? It’s not. Because most of what you eat is loaded with these minerals without you even knowing it.
Sodium: The Hidden Culprit
You might think you’re eating clean because you skip the salt shaker. But 75% of sodium in the average diet comes from processed and packaged foods-canned soups, frozen meals, deli meats, bread, and even breakfast cereals. A single serving of canned soup can have 800-1,200 mg of sodium. That’s almost half your daily limit before you even start cooking.
Reading labels is non-negotiable. Look for “sodium” on the nutrition facts. Avoid anything with more than 140 mg per serving-that’s considered low-sodium by FDA standards. Choose “no salt added” or “unsalted” versions. Use herbs like rosemary, thyme, or garlic powder instead of salt. Mrs. Dash or similar blends work well because they add flavor without sodium. Cutting sodium by just 1,000 mg a day can lower your systolic blood pressure by 5-6 mmHg, which reduces strain on your kidneys and heart.
Potassium: The Tricky Balance
Potassium is found in almost every healthy food-bananas, oranges, potatoes, spinach, tomatoes, beans, and avocados. But for someone with kidney disease, these are risky. A medium banana has 422 mg of potassium. One cup of cooked spinach? 840 mg. That’s more than your daily limit in one meal.
Here’s the trick: not all potassium is the same. Potassium from animal sources like meat and dairy is absorbed at 80-90%, while plant-based potassium is only 50-70% absorbed. That means you can sometimes eat more vegetables than meat and still stay safe. But portion control is key. A half-cup of cooked cabbage has just 12 mg of potassium. A half-cup of blueberries? 65 mg. Apples? 150 mg per medium fruit. These are your friends.
Leaching is a game-changer. If you love potatoes or carrots, soak them in warm water for 2-4 hours, then boil them in a large amount of water (at least 5 cups). This can cut potassium by up to 50%. DaVita’s 2023 nutrition guide confirms this method works. Swap white bread (60 mg phosphorus per slice) for whole grain (150 mg). Swap bananas for apples. Swap orange juice for apple juice. Small swaps add up.

Phosphorus: The Silent Threat
Phosphorus is where things get complicated. There’s natural phosphorus in foods like dairy, meat, and nuts-and then there’s added phosphorus in processed foods. The difference? Your body absorbs nearly 100% of the added kind, but only 50-70% of the natural kind.
That means a slice of processed cheese can have 250 mg of phosphorus, while a half-cup of milk has only 125 mg. A 12-ounce cola? 450 mg. That’s almost half your daily limit in one drink. Even “diet” colas have phosphorus additives. Avoid them.
Look for ingredients with “phos” in them: phosphoric acid, sodium phosphate, calcium phosphate. These are red flags. Choose fresh meats over processed ones. Skip deli meats, hot dogs, and pre-marinated chicken. Go for plain, unseasoned fish like cod or halibut-2-3 ounces, two to three times a week. It’s low in sodium and manageable in phosphorus and potassium.
What You Can Still Eat
Yes, you can still enjoy meals that feel satisfying. Here’s a simple guide:
- Grains: White bread, white rice, pasta (not whole grain)
- Fruits: Apples, berries, grapes, pineapple, watermelon
- Veggies: Cabbage, cauliflower, green beans, onions, peppers
- Proteins: Egg whites, skinless chicken breast, unsalted fish (cod, tilapia, halibut)
- Dairy: Small portions of milk (½ cup), unprocessed cheese (1 oz)
- Fats: Olive oil, butter (in moderation), light mayonnaise
Portion sizes matter. Even low-potassium foods can push you over if you eat too much. A half-cup of blueberries is fine. A whole pint? Not so much.
Fluids and Other Considerations
If your kidneys aren’t making much urine-less than 1 liter a day-you’ll also need to limit fluids. That includes water, tea, coffee, soup, ice cream, and even gelatin. Most patients are told to stick to 32 ounces (1 liter) a day. Use a small cup to measure. Keep a log. It helps you stay on track.
Protein intake needs attention too. Old advice said to eat as little protein as possible. But new research shows that’s dangerous. Eating too little protein increases malnutrition risk by 34% in older adults with CKD. The updated KDOQI 2020 guidelines recommend 0.55-0.8 grams of high-quality protein per kilogram of body weight. That means a 70 kg (154 lb) person needs about 38-56 grams of protein daily. Egg whites, lean meats, and fish are best.
Real Challenges and How to Beat Them
Most people struggle with potassium first. Healthy eating guides tell you to eat more fruits and veggies-but for you, that’s risky. It’s frustrating. You’re not being lazy. You’re trying to follow advice that doesn’t fit your body.
Meal planning takes time. Start simple. Pick one meal a day to plan. Make a list of 5 safe breakfasts, 5 lunches, and 5 dinners. Rotate them. Use apps like Kidney Kitchen, which has been downloaded over 250,000 times and tracks nutrients in real time. Some patients take 3-6 months to adjust. That’s normal.
Medicare now covers 3-6 sessions per year with a renal dietitian for stage 4 CKD patients. If you haven’t seen one, ask your doctor. They’ll help you personalize your plan. No two kidneys are the same. Your blood tests, age, other conditions, and even your gut bacteria affect how your body handles minerals.
The Bigger Picture
A well-managed renal diet doesn’t just prevent emergencies. It buys you time. Research from Columbia University shows that proper diet can delay the need for dialysis by 6-12 months in stage 4 CKD. That’s more time with family, fewer hospital visits, and better quality of life.
And it’s not just about restriction. It’s about smart choices. Choosing white bread over whole grain isn’t giving up-it’s protecting your body. Avoiding cola isn’t being deprived-it’s preventing heart damage. Eating a small portion of apple instead of a banana isn’t boring-it’s keeping your heart safe.
There’s no perfect diet. But there’s a diet that works-for you. It’s not about perfection. It’s about consistency. Small changes, day after day, make all the difference.
Can I still eat fruits and vegetables on a renal diet?
Yes, but you need to choose carefully and control portions. Low-potassium options include apples, berries, cabbage, cauliflower, and green beans. Soaking and boiling high-potassium veggies like potatoes or carrots can reduce their potassium by up to 50%. Avoid bananas, oranges, tomatoes, spinach, and avocados unless you’re under close medical supervision.
Is salt the only source of sodium in my diet?
No. About 75% of sodium comes from processed and packaged foods-canned soups, frozen meals, deli meats, bread, and snacks. Even foods that don’t taste salty, like cereal or cheese, can be high in sodium. Always check nutrition labels for sodium content per serving. Look for "no salt added" or "low sodium" options.
Why should I avoid colas and processed cheese?
Colas contain phosphoric acid, which adds 450 mg of phosphorus per 12-ounce can. Processed cheese has added phosphorus compounds like sodium phosphate, which your body absorbs almost completely-up to 90-100%. This leads to dangerous phosphorus buildup, which can harden blood vessels and weaken bones. Stick to fresh, unprocessed foods.
Do I need to limit protein on a renal diet?
Not as much as you might think. While very high protein intake can stress kidneys, too little protein causes muscle loss and malnutrition, especially in older adults. The current guideline recommends 0.55-0.8 grams of high-quality protein per kilogram of body weight daily. Focus on egg whites, fish, and skinless chicken. Avoid processed meats like sausages and deli slices.
Can I use herbs and spices instead of salt?
Absolutely. Herbs like basil, oregano, and rosemary, and spice blends like Mrs. Dash, add flavor without sodium. Avoid salt substitutes that contain potassium chloride-they can raise potassium levels dangerously. Always check labels on spice blends to make sure they’re sodium-free and potassium-free.
How do I know if my diet is working?
Your blood tests tell the story. Regular checks for sodium, potassium, phosphorus, and calcium levels show whether your diet is effective. If potassium stays below 5.0 mEq/L, phosphorus under 1000 mg/dL, and sodium is controlled, you’re on track. Also, watch for swelling, shortness of breath, or muscle cramps-these can signal imbalances. Keep a food log and share it with your dietitian.
Are there any new developments in renal dieting?
Yes. The FDA approved the first medical food for CKD, Keto-1, in 2023, which provides essential nutrients while minimizing phosphorus and potassium. New research also shows that prebiotic fibers like inulin may reduce phosphorus absorption by 15-20%. Apps that sync with your lab results are being piloted at places like Mayo Clinic, offering real-time dietary adjustments based on your body’s needs.
Can I follow a renal diet if I also have diabetes?
It’s challenging but possible. About 44% of new kidney disease cases come from diabetes. The problem? Heart-healthy foods for diabetics-like whole grains, beans, and citrus fruits-are often high in potassium or phosphorus. Work with a renal dietitian who also understands diabetes. Focus on low-potassium fruits (apples, berries), white rice instead of brown, and lean proteins. Portion control and timing are critical.



