When a stomach‑ache throws a wrench into your day, you instinctively reach for an acid‑reducing medication. Ranitidine is a once‑popular H2‑blocker that was pulled from shelves worldwide after concerns about NDMA contamination. If you’ve been using ranitidine or heard about it in the news, you’re probably asking: what are the safe, effective ranitidine alternatives and how do they stack up?
Quick Take
- Ranitidine was withdrawn in 2020 due to potential carcinogen NDMA.
- Modern H2‑blockers (famotidine, cimetidine, nizatidine) work similarly but have cleaner safety records.
- Proton‑pump inhibitors (PPIs) such as omeprazole and pantoprazole are stronger but may need longer‑term monitoring.
- Choice depends on symptom severity, dosing convenience, and any existing medical conditions.
What Raniten Actually Did
Ranitidine belongs to the H2‑receptor antagonist class. By blocking histamine‑2 receptors on gastric parietal cells, it reduces the amount of hydrochloric acid released. Typical over‑the‑counter doses were 75mg twice daily or 150mg once daily, with an onset of relief within 30‑60minutes.
The drug’s downfall wasn’t because it stopped working-it was the discovery of N‑nitrosodimethylamine (NDMA), a probable human carcinogen, forming in some batches under normal storage conditions. Regulators in the US, EU, and Canada issued recalls, and manufacturers voluntarily halted production.
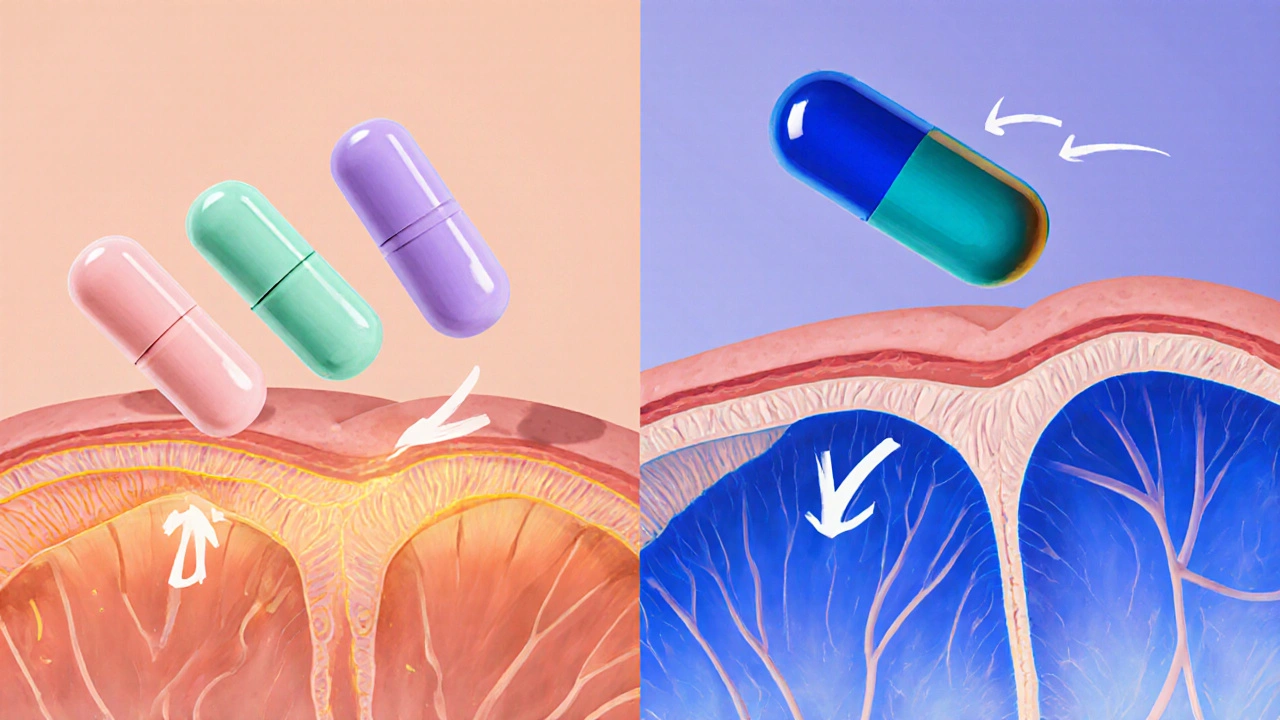
Modern H2‑Blockers: Direct Substitutes
If you liked the quick‑acting profile of ranitidine, the safest modern H2‑blockers are:
- Famotidine - 20mg twice daily for heartburn; 40mg once daily for ulcer prevention. Onset: 30minutes. Lower risk of drug‑drug interactions.
- Cimetidine - 200mg twice daily. Effective but can interfere with hepatic enzymes, raising levels of certain medications.
- Nizatidine - 150mg once daily. Similar potency to ranitidine, rarely used in the US.
All three share the same mechanism as ranitidine but have been vetted for NDMA formation, making them reliable stand‑ins.
Proton‑Pump Inhibitors: The Stronger Contenders
When occasional heartburn isn’t the only problem-think erosive esophagitis, Barrett’s esophagus, or chronic NSAID use-PPIs provide a more robust acid suppression. The most common PPIs are:
- Omeprazole - 20mg once daily; onset 1‑2hours; effective for severe GERD.
- Pantoprazole - 40mg once daily; minimal drug interactions; often chosen for patients on multiple meds.
- Esomeprazole - 20‑40mg once daily; marketed as “Nexium,” slightly higher bioavailability.
- Lansoprazole - 15‑30mg once daily; good for healing gastric ulcers.
PPIs inhibit the H+/K+ ATPase pump-the final step in acid production-so they achieve a deeper, longer‑lasting pH rise than H2‑blockers. The downside? They can increase risk of vitamin B12 deficiency, magnesium loss, and Clostridioides difficile infection when used beyond 8 weeks.
Side‑Effect Snapshot: H2‑Blockers vs PPIs
| Drug Class | Typical Side‑Effects | Serious Risks (Long‑Term) |
|---|---|---|
| H2‑Blockers (Famotidine, Cimetidine, Nizatidine) | Headache, dizziness, mild diarrhea | Rare hepatic enzyme interaction (cimetidine), minimal nutrient impact |
| PPIs (Omeprazole, Pantoprazole, Esomeprazole, Lansoprazole) | Upper‑abdominal pain, flatulence, nausea | Bone fracture risk, B12 deficiency, increased infection rates |
How to Pick the Right Alternative
Think of your decision like matching a shoe to an outfit. Consider three main factors:
- Symptom intensity. Mild heartburn? An H2‑blocker works fast and can be taken as needed. Persistent reflux? A PPI may be more effective.
- Medication profile. If you’re on warfarin, antidepressants, or anticonvulsants, choose famotidine (few interactions) over cimetidine.
- Duration of therapy. For short‑term relief (<2 weeks), H2‑blockers suffice. For chronic conditions, discuss a step‑down plan-start with a PPI, then switch to an H2‑blocker once inflammation improves.
Consult your healthcare provider before swapping, especially if you have kidney disease, liver impairment, or are pregnant.
Switching Safely: A Practical Checklist
- Confirm your diagnosis (heartburn, ulcer, GERD) with a clinician.
- Identify current dose and timing of ranitidine.
- Select an alternative matching your dosing convenience (once‑daily famotidine vs twice‑daily cimetidine).
- Review potential interactions using a reliable drug‑interaction tool.
- Start the new drug at the recommended dose; if symptoms persist after 7‑10 days, contact your doctor.
- Track side‑effects in a simple journal-note any new headaches, stomach pain, or unusual fatigue.
Frequently Asked Questions
Is famotidine as safe as ranitidine?
Yes. Famotidine underwent extensive testing and showed no NDMA formation, making it the go‑to H2‑blocker after ranitidine’s withdrawal.
Can I take a PPI and an H2‑blocker together?
Sometimes doctors prescribe a PPI for night‑time control and an H2‑blocker for breakthrough heartburn. However, timing matters-take the H2‑blocker at least two hours apart from the PPI to avoid reduced effectiveness.
What’s the fastest‑acting alternative?
Famotidine works within 30 minutes, matching ranitidine’s speed. If you need immediate relief, chewable antacids (e.g., calcium carbonate) act in minutes but don’t provide lasting suppression.
Are PPIs safe for long‑term use?
Long‑term PPI therapy is generally safe when monitored. Annual labs for magnesium and B12, plus bone density checks after 2‑3 years, help catch rare deficiencies early.
What should I do if I experience rebound acid hypersecretion after stopping a PPI?
Taper the PPI over 2‑4 weeks while adding a low‑dose H2‑blocker (famotidine 10mg nightly). This softens the rebound effect and eases the transition.




Michael Dennis, October 2, 2025
While the article adequately outlines the distinction between H2‑blockers and PPIs, it ultimately fails to delve into the nuanced pharmacokinetic profiles that might influence a clinician's choice. The omission of detailed absorption rates, for instance, leaves a gap for readers seeking a deeper understanding.
Blair Robertshaw, October 5, 2025
Honestly, this piece is a dumpster fire of half‑baked advice. It rly pretends to be thorough but ends up spitting out generic lists that any 5‑year‑old on the internet could copy‑paste. The author forgets to mention that famotidine can actually cause headaches for some folks, which is an important side‑effect to track.
Alec Maley, October 8, 2025
Hey everyone, totally get the confusion after the ranitidine recall – it’s a lot to take in. If you’re looking for something that works fast without the NDMA worries, famotidine is a solid pick. It kicks in within half an hour, and most people tolerate it well, so you can get back to your day quicker.
Navjot Ghotra, October 9, 2025
Just a heads up famotidine works fast no biggie it’s cheap and safe enough for most people who need quick relief.
Claus Rossler, October 12, 2025
One might argue that the prevailing consensus glorifies PPIs as the universal remedy, yet such a monolithic view neglects the elegance of H2‑blockers. A discerning practitioner should recognize that, while PPIs achieve deeper acid suppression, they also usher in a cascade of metabolic perturbations that merit caution.
chris mattox, October 14, 2025
Let’s paint the bigger picture, folks: swapping ranitidine for famotidine isn’t just a cookie‑cutter decision. Think of it like swapping a bland broth for a vibrant stew – the flavors, interactions, and side‑effects all shift. Embrace the change, and you’ll find a more harmonious gut environment.
Jackson Whicker, October 16, 2025
In the grand theater of gastro‑pharmacology, the choice between an H2‑blocker and a proton‑pump inhibitor mirrors a philosophical duel between immediacy and profundity. To favor the swift, measurable antagonism of famotidine is to celebrate the virtue of restraint, whereas surrendering to the all‑encompassing suppression of omeprazole may betray a hubristic desire to dominate the acid frontier.
Audrin De Waal, October 17, 2025
Look, here’s the deal – the global health community keeps pushing PPIs like they’re the only answer, but that’s just western pharma hype. In our own backyard, we’ve seen patients thrive on simple H2‑blockers without the pricey side‑effects. Don’t let big‑drug narratives dictate your gut health.
parag mandle, October 19, 2025
From a clinical standpoint, the transition away from ranitidine should be guided by both efficacy and safety data. Famotidine, for example, exhibits a lower propensity for cytochrome‑P450 inhibition, which reduces drug‑drug interaction risks-a crucial consideration for polypharmacy patients. Moreover, its pharmacodynamic profile provides rapid symptom relief comparable to ranitidine, making it a seamless substitute for most indications.
Shivali Dixit Saxena, October 21, 2025
Quick tip: take famotidine with food.
Sayam Masood, October 22, 2025
One could perceive the recommendation to pair famotidine with meals as a mere procedural note, yet it subtly underscores the interplay between gastric pH modulation and nutrient absorption-a relationship that, when understood, refines therapeutic outcomes.
Jason Montgomery, October 24, 2025
Alright team, remember that you’re not alone in navigating these meds. If you try famotidine and notice lingering heartburn, give it a few days – sometimes the body just needs time to adjust. Stay patient, stay hydrated, and you’ll get through this.
Wade Developer, October 27, 2025
The dialectic between acid suppression potency and systemic ramifications invites a measured appraisal. While PPIs dominate the therapeutic hierarchy in severe gastro‑oesophageal reflux disease, the incremental risk profile they introduce necessitates judicious, time‑bounded prescriptions to preserve physiological equilibrium.
Sandra Perkins, October 28, 2025
Oh great, another “must‑read” guide. As if we needed more boilerplate advice.
rama andika, October 29, 2025
Sure, the article says PPIs are “stronger,” but have you considered that big pharma might be sprinkling hidden nano‑chips in those pills to monitor our digestion? Stay vigilant, friends. The truth is rarely what the label says.
Kenny ANTOINE-EDOUARD, November 1, 2025
When evaluating alternatives to ranitidine, it is essential to adopt a systematic approach that accounts for pharmacological efficacy, safety profile, drug‑interaction potential, and patient‑specific factors. First, consider the onset of action; famotidine, for instance, reaches peak plasma concentration within 1‑2 hours, offering rapid symptomatic relief comparable to the former ranitidine regimen. Second, assess the metabolic pathway: famotidine is renally excreted largely unchanged, thereby minimizing hepatic enzyme involvement and reducing the risk of adverse interactions with concomitant medications such as warfarin or certain antidepressants. Third, examine the side‑effect spectrum. While H2‑blockers generally present mild adverse events like headache or dizziness, PPIs have been associated with long‑term complications, including hypomagnesemia, vitamin B12 deficiency, and increased susceptibility to enteric infections. Fourth, weigh the duration of therapy; H2‑blockers are suitable for intermittent, as‑needed use, whereas PPIs often require a structured tapering protocol to avoid rebound acid hypersecretion. Fifth, incorporate patient comorbidities into the decision matrix. Individuals with chronic kidney disease or reduced renal function may require dose adjustments of famotidine, whereas those with osteoporosis may be better served by avoiding prolonged PPI exposure. Sixth, consider cost and accessibility; famotidine is widely available over the counter at a modest price point, while some PPIs may be subject to insurance formularies or higher out‑of‑pocket costs. Finally, engage patients in shared decision‑making, providing clear education on the expected timeline for symptom improvement and potential risks associated with each therapeutic class. By meticulously integrating these eight considerations, clinicians can tailor acid‑reducing therapy to each patient’s unique clinical context, thereby optimizing outcomes while mitigating unnecessary hazards.
Craig Jordan, November 3, 2025
It is a curious phenomenon that, despite the extensive body of literature extolling the virtues of proton‑pump inhibitors, many practitioners persist in prescribing them as first‑line agents for even the most benign cases of heartburn. One must ask why this paradigm persists. Is it merely a matter of habit, or does the pharmaceutical industry’s subtle nudging play a role? Indeed, the allure of a once‑daily dose that promises near‑complete acid suppression may appear seductive, yet the downstream consequences – ranging from altered gut microbiota to impaired calcium absorption – are often glossed over in clinical summaries. Moreover, the economic incentives embedded within drug formularies cannot be ignored; the higher reimbursement rates associated with PPIs compared to H2‑blockers create a systemic bias that subtly shapes prescribing behavior. In parallel, the narrative that H2‑blockers are “older” and therefore inferior fails to recognize the modern advancements in drug design that have yielded agents such as famotidine, which demonstrate a favorable safety profile and robust efficacy. Consequently, a re‑evaluation of treatment algorithms is warranted, one that privileges patient‑centered outcomes over pharmaceutical convenience. By critically appraising the evidence and disentangling it from commercial influences, clinicians can make more nuanced decisions that align with the best interests of their patients, rather than defaulting to the path of least resistance.
Jeff Quihuis-Bell, November 5, 2025
Listen up, friends! If you’re wrestling with that post‑ranitidine void, grab a bottle of famotidine and give it a whirl. It’s quick, it’s cheap, and it won’t have you worrying about mysterious contaminants. Keep an eye on how you feel, stay hydrated, and you’ll bounce back faster than you think.
Jessica Tang, November 7, 2025
For anyone still on the fence about switching, remember that the choice ultimately hinges on your personal health profile. If you have minimal comorbidities and need occasional relief, an H2‑blocker like famotidine may serve you well. Conversely, if you’re dealing with severe reflux or esophagitis, a short course of a PPI could be justified, provided you monitor for potential side‑effects.