Copegus is not a cure-all, but for people with chronic hepatitis C, it’s been a lifeline for over two decades. It doesn’t work alone. It doesn’t promise quick results. But when paired with the right other drugs, it helps clear the hepatitis C virus from the body - and that’s something millions have achieved because of it.
What Copegus Actually Is
Copegus is the brand name for ribavirin, an antiviral drug first approved in the late 1990s. It’s not like a painkiller or an antibiotic. You don’t take it to feel better right away. Instead, it attacks the genetic material of the hepatitis C virus, making it harder for the virus to multiply. Think of it like scrambling the copy machine the virus uses to make more copies of itself.
The active ingredient, ribavirin, has been around since the 1970s. It was originally tested for other viruses, but its real breakthrough came when doctors started using it with interferon - and later, with direct-acting antivirals (DAAs). Today, Copegus is rarely used alone. It’s almost always part of a combo treatment plan.
How Copegus Works in the Body
When you swallow a Copegus tablet, your body breaks it down into its active form. From there, it gets absorbed into your bloodstream and travels to your liver - where the hepatitis C virus hangs out. Once there, ribavirin interferes with the virus’s RNA replication. It doesn’t kill the virus outright. Instead, it causes so many errors in the virus’s genetic code that it can’t survive long enough to infect new cells.
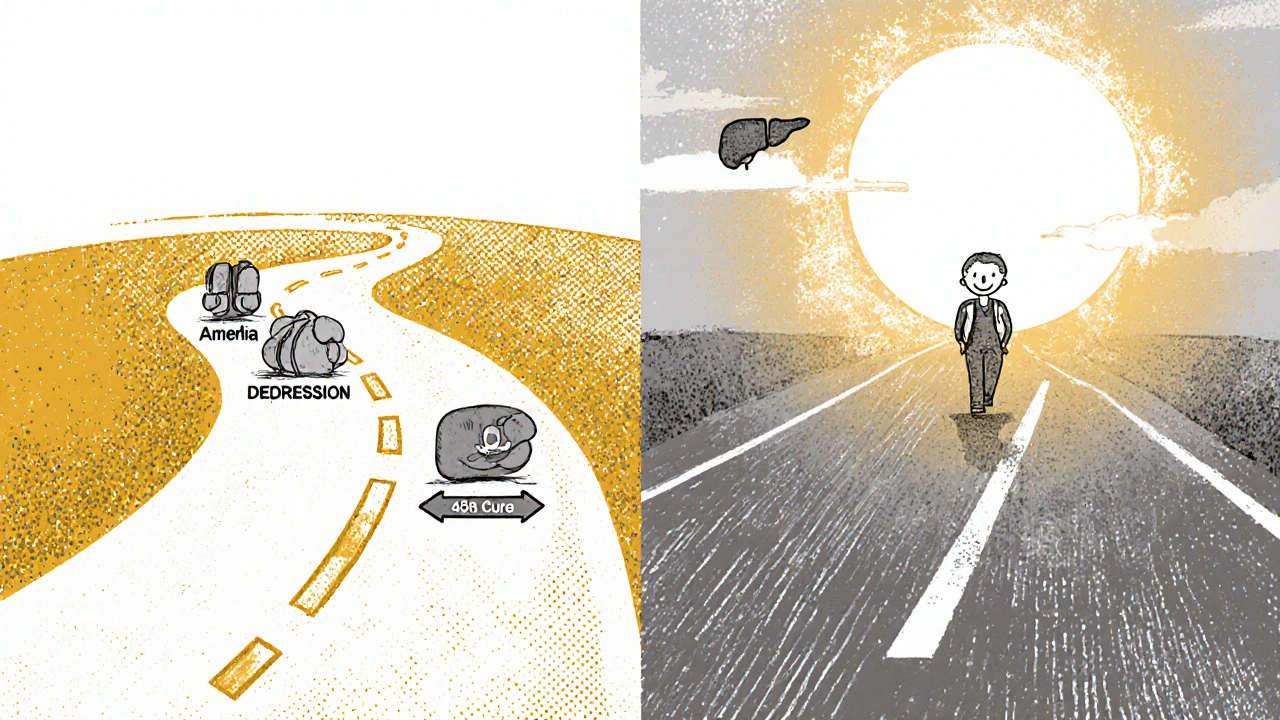
This is why Copegus needs time. You can’t take it for three days and expect results. Treatment usually lasts 24 to 48 weeks, depending on the hepatitis C genotype and whether you’ve been treated before. The goal isn’t symptom relief - it’s viral clearance. Blood tests after treatment show whether the virus is undetectable. That’s called a sustained virologic response (SVR), and it means you’re cured.
Who Copegus Is Prescribed For
Copegus isn’t for everyone with hepatitis C. Since 2014, newer direct-acting antivirals like sofosbuvir and daclatasvir have become the first-line treatment. They’re more effective, have fewer side effects, and don’t require injections.
So why still use Copegus? Three main reasons:
- Genotype 3 infection - especially if the patient has cirrhosis
- Patients who can’t afford newer DAAs
- Those who’ve failed previous treatments and need a backup option
In the UK, NICE guidelines recommend Copegus only in specific cases now. It’s mostly used in resource-limited settings or when newer drugs aren’t accessible. In the US, it’s still sometimes used in combination with pegylated interferon for genotype 1 or 4 in patients with advanced liver disease who can’t tolerate newer therapies.
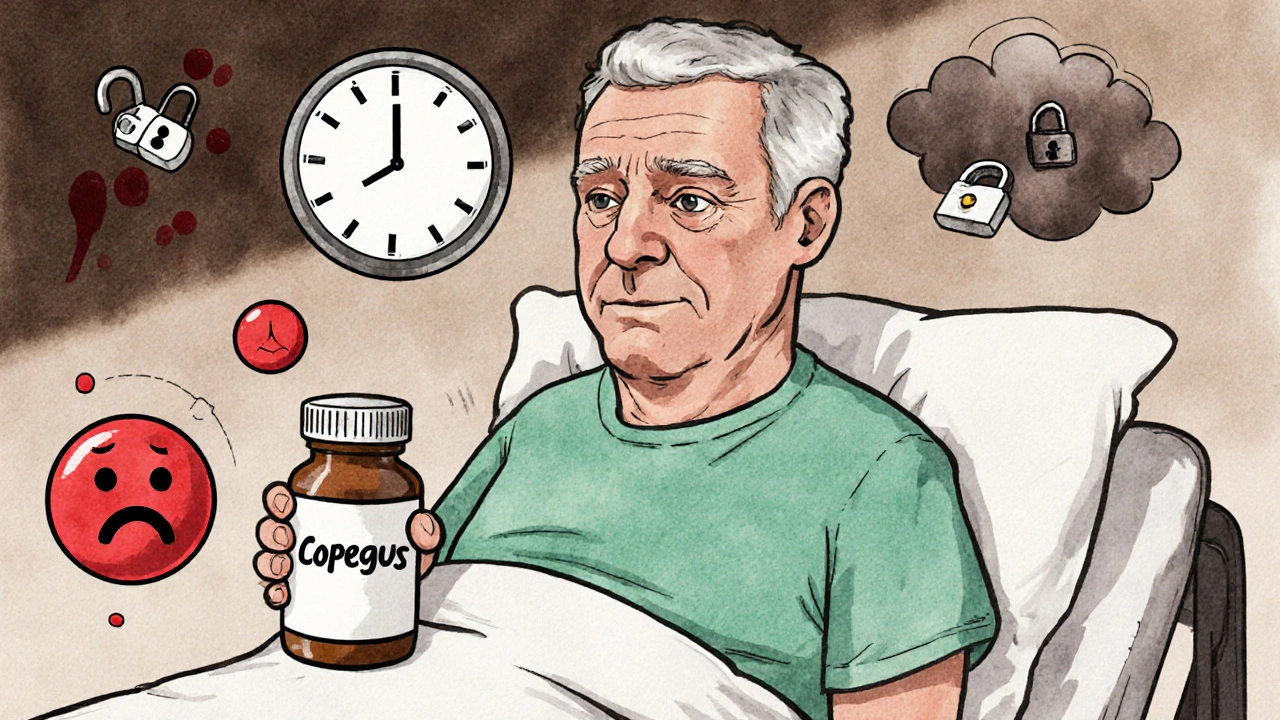
Side Effects You Can’t Ignore
Copegus isn’t gentle. It’s one of the toughest antivirals you can take. About 80% of people on Copegus experience side effects. Some are mild. Others are serious.
Common side effects include:
- Severe fatigue
- Anemia (low red blood cells - this is the most frequent reason people need dose reductions)
- Headaches and dizziness
- Insomnia
- Depression and mood swings
- Dry skin and itching
- Loss of appetite and weight loss
The anemia isn’t just annoying - it’s dangerous. Ribavirin destroys red blood cells. Doctors monitor hemoglobin levels every week during treatment. If levels drop too low, they reduce the dose or stop Copegus entirely. Some patients need blood transfusions.
It also causes birth defects. That’s why both men and women must use two forms of birth control during treatment and for six months after stopping. Pregnancy tests are required monthly for women of childbearing age.
How Copegus Compares to Other Hepatitis C Treatments
| Treatment | Duration | Success Rate (SVR) | Main Side Effects | Cost (UK estimate) |
|---|---|---|---|---|
| Copegus + Peginterferon | 24-48 weeks | 40-70% | Anemia, depression, flu-like symptoms | £1,500-£3,000 |
| Sofosbuvir + Ledipasvir | 8-12 weeks | 95-99% | Mild headache, fatigue | £20,000-£30,000 |
| Daclatasvir + Sofosbuvir | 12 weeks | 94-98% | Headache, nausea | £18,000-£28,000 |
| Elbasvir/Grazoprevir | 12 weeks | 95-98% | Fatigue, rash | £22,000-£32,000 |
The numbers speak for themselves. Newer drugs cure more people in less time with far fewer side effects. But they’re expensive. In places where healthcare systems can’t afford them, Copegus remains a practical, if harsh, alternative.
What Happens If You Stop Copegus Early
Skipping doses or quitting treatment early doesn’t just mean the virus comes back - it makes future treatment harder. The hepatitis C virus mutates quickly. If you don’t fully eliminate it, surviving strains become resistant to drugs. That’s called treatment failure. And once you’ve failed a regimen, your options shrink.
People who stop Copegus because of side effects often feel guilty. But doctors understand. If your hemoglobin drops below 8.5 g/dL, or if depression becomes overwhelming, your doctor will adjust your dose or switch you to a different plan. There’s no shame in changing course. What matters is finishing treatment safely.
Real-Life Experience: A Patient’s Story
In 2023, a 52-year-old man from Leeds was diagnosed with genotype 3 hepatitis C and cirrhosis. He couldn’t get the newest DAAs through the NHS due to funding restrictions. His doctor offered him Copegus with peginterferon. He took it for 48 weeks.
He lost 15 pounds. He needed two blood transfusions. He cried on the phone with his daughter every other week because he was too tired to play with his grandkids. But after six months of treatment, his viral load dropped to undetectable. One year later, his liver enzymes returned to normal. He’s still alive. He’s still working. He didn’t get cured because the treatment was easy. He got cured because he stuck with it.
When Copegus Isn’t an Option
Some people simply can’t take Copegus. It’s not safe if you have:
- Severe heart disease
- Autoimmune liver disease
- Severe kidney impairment
- History of suicidal thoughts or severe depression
- Pregnancy or plans to conceive in the next six months
If you have any of these, your doctor will look at alternatives. Sometimes that means waiting for access to newer drugs. Sometimes it means clinical trials. Sometimes it means palliative care. But there’s always a path - even if it’s not the one you hoped for.
What to Do If You’re Prescribed Copegus
If your doctor says Copegus is right for you, here’s what to do:
- Get a full blood panel before starting - check hemoglobin, kidney and liver function.
- Ask about financial support. Some charities help cover the cost.
- Set up weekly check-ins with your nurse or doctor.
- Keep a symptom journal - note fatigue, mood, appetite, sleep.
- Don’t take any other medications without checking with your doctor - Copegus interacts with many drugs.
- Use two forms of birth control. Always.
- Stay connected. Isolation makes side effects worse. Talk to someone - a support group, a friend, a counselor.
It’s not a glamorous treatment. But for some, it’s the only shot at a cure. And that’s worth fighting for.
Is Copegus still used today?
Yes, but only in specific cases. It’s mostly used today for genotype 3 hepatitis C with cirrhosis, or when newer direct-acting antivirals aren’t available due to cost or access issues. In most high-income countries, it’s no longer first-line treatment.
Can Copegus cure hepatitis C on its own?
No. Copegus alone doesn’t reliably clear hepatitis C. It only works when combined with other antivirals - historically with interferon, and sometimes with newer drugs like sofosbuvir in specific cases. Always take it as part of a prescribed combination.
How long does Copegus treatment last?
Treatment usually lasts between 24 and 48 weeks, depending on your hepatitis C genotype, liver condition, and whether you’ve been treated before. Your doctor will determine the exact length based on your individual case.
What are the biggest risks of taking Copegus?
The biggest risks are severe anemia, depression, and birth defects. Anemia can require blood transfusions. Depression can become life-threatening. And if you or your partner get pregnant during or after treatment, the baby could be born with serious physical abnormalities. Strict birth control and mental health monitoring are mandatory.
Can I drink alcohol while taking Copegus?
No. Alcohol puts extra stress on your liver - the very organ fighting the hepatitis C virus. Drinking while on Copegus can speed up liver damage and reduce your chances of cure. Complete abstinence is required during treatment and for at least six months after.
Are there cheaper alternatives to Copegus?
Generic ribavirin is available in many countries at a fraction of the brand-name cost. In the UK, the NHS may cover newer DAAs for most patients now, making Copegus less common. If cost is an issue, talk to your doctor about patient assistance programs or generic options.
Final Thoughts
Copegus is a relic of an older era of hepatitis C treatment - but it’s not obsolete. For some, it’s still the only way out. It’s hard. It’s painful. It changes your life. But for those who finish the course, it can mean the difference between a future with liver failure and a future with normal life expectancy.
If you’re on Copegus, you’re not just taking a pill. You’re fighting a silent disease with everything you’ve got. And that deserves respect - not pity.




Saket Sharma, November 18, 2025
Copegus? That’s a relic. Ribavirin’s a blunt instrument-hemoglobin drops like a rock, and you’re stuck with flu-like agony for a year. Modern DAAs cure in 8 weeks with zero drama. If your doc still pushes this, they’re stuck in 2010.
Genotype 3 with cirrhosis? Even then, sofosbuvir/velpatasvir is the real play. Stop clinging to the past.
And don’t even get me started on the birth control rules. It’s not a suggestion. It’s a legal requirement. One mistake, and you’re ruining a life.
Stop romanticizing suffering. This isn’t war. It’s medicine.
Alex Boozan, November 19, 2025
Let’s be real-Copegus is what happens when your country can’t afford real treatment. In the US, we don’t need this garbage. We’ve got cure rates over 95% with pills you take once a day.
Anyone still using interferon + ribavirin is either in a developing country or their insurance is broken. Either way, it’s a national disgrace that people are still getting this treatment in 2025.
And yes, the anemia is brutal. I’ve seen patients need transfusions. That’s not treatment. That’s torture with a prescription.
Stop glorifying suffering. We have better tools. Use them.
mithun mohanta, November 19, 2025
Look, I get it-Copegus is the ‘poor man’s cure,’ but let’s not pretend it’s noble. Ribavirin? It’s like throwing sand into a jet engine and hoping it stops. The side effects? A full-time job.
And don’t even get me started on the ‘two forms of birth control’ rule-because, of course, the virus doesn’t discriminate, but your uterus? Oh, it’s a liability.
Meanwhile, in India, generics are selling for $20 a month. Why are we still talking about this like it’s a heroic choice? It’s not. It’s a stopgap. A Band-Aid on a hemorrhage.
And yes-I’m saying this with my hemoglobin at 8.2 last year. I know. I lived it. It’s not ‘courage.’ It’s desperation dressed in medical jargon.
Stop calling it ‘a lifeline.’ It’s a life sentence with extra steps.
And the fatigue? Oh, the fatigue. You don’t sleep. You just… exist. Like a ghost with a pill organizer.
And yes-I cried too. Every. Single. Week.
But hey-at least I’m alive. So… congrats? I guess?
Still. We can do better.
And we will.
Because we have to.
Evan Brady, November 21, 2025
Let me break this down like I’m explaining it to a friend who just got diagnosed: Copegus isn’t the star-it’s the supporting actor. The real heroes are the DAAs. Ribavirin? It’s the wingman who shows up with a bad haircut and smells like burnt coffee.
It works by sabotaging the virus’s copy machine-like tossing glitter into a photocopier until every page comes out as abstract art. The virus can’t replicate. It starves. It fades.
But here’s the kicker: it doesn’t just attack the virus. It attacks your red blood cells. That’s why your hemoglobin tanks. That’s why you’re exhausted. That’s why your doctor checks your blood every week like a hawk.
And yes, it’s brutal. But here’s what no one says: it’s also *effective*. In places where a $1000 pill is a fantasy, Copegus + interferon is the difference between a funeral and a birthday party.
It’s not pretty. It’s not elegant. But it’s honest. And sometimes, honesty is the only thing that keeps you alive.
Also-don’t drink. Ever. Not even a sip. Your liver is already on life support. Alcohol is the unplugged cord.
And if you’re on this regimen? You’re not broken. You’re a warrior. Quietly. Without fanfare. Just grinding. And that’s worth more than any viral load number.
Ram tech, November 21, 2025
copegus? lol. why even use it? new drugs are 99% cure and no anemia. who still uses this? old docs? broke countries? guess im lucky i live in usa. just take the pill, chill, done in 2 months. why suffer? 🤡
Jenny Lee, November 22, 2025
My cousin did Copegus for 48 weeks. Lost 20 lbs. Needed two transfusions. Still smiled every morning. She didn’t talk about it much. Just showed up. That’s the quiet strength no one writes about.
Don’t call it outdated. Call it necessary.
Jeff Hakojarvi, November 23, 2025
Just wanted to say-if you’re reading this and you’re on Copegus right now, I see you.
I’ve been there. The fatigue isn’t just ‘tired.’ It’s like your bones are filled with wet cement.
And the anemia? Yeah, it’s scary. But your medical team is watching you. They’re not ignoring you.
Keep that symptom journal. Even if you write ‘felt like crying today’-that counts. It’s data. It’s proof you’re still fighting.
And if you’re thinking about quitting because it’s too hard? Talk to your nurse first. Dose adjustments exist. You don’t have to suffer in silence.
You’re not weak for needing help. You’re strong for showing up.
And if you’re reading this and you’re not on it? Don’t judge. Some people don’t get to choose the easy path. And that doesn’t make their fight any less valid.
You’re not alone. I’m right here with you.
One day at a time.
One pill at a time.
Timothy Uchechukwu, November 24, 2025
Why do Americans think they own the cure? In Nigeria we use Copegus because we don’t need your overpriced pills. We know what works. Your fancy DAAs are a scam. Big Pharma invented them to make money. Ribavirin has been saving lives for 30 years. You don’t need a $30k pill to beat a virus. You need willpower. And we have it.
Stop acting like you’re better because you have insurance. We’re curing people with $5 pills and no doctors. You call that backward. We call it real.