When you’re scheduled for a CT scan or X-ray with contrast dye, the last thing you want to worry about is having a reaction. But if you’ve had one before-or even if you’re just nervous-knowing what to expect and how to prepare can make all the difference. The truth is, serious reactions to contrast dye are rare, but they’re not impossible. And for people with a history of reactions, the risk of having another one jumps up dramatically. That’s where pre-medication and safety planning come in.
What Counts as a Contrast Dye Reaction?
Contrast dye, usually iodinated, helps doctors see blood vessels, organs, and tissues more clearly during imaging. Most people tolerate it just fine. But some have reactions. These aren’t true allergies like peanut or penicillin allergies. They’re called anaphylactoid reactions-they look like allergies, but they’re triggered differently by the body’s response to the chemical. Reactions fall into three buckets:- Mild: Itching, mild rash, nausea, or a warm flush. These happen in about 1 in 100 people and usually go away on their own.
- Moderate: More intense vomiting, hives, swelling, or wheezing. These need treatment but aren’t life-threatening.
- Severe: Low blood pressure, trouble breathing, cardiac arrest. These are rare-about 1 in 2,500 to 1 in 10,000 scans-but can be deadly if not handled fast.
Here’s the key: if you’ve had a moderate or severe reaction before, your chance of having another one is around 35%. That’s why pre-medication exists-to slash that risk.
Who Needs Pre-Medication?
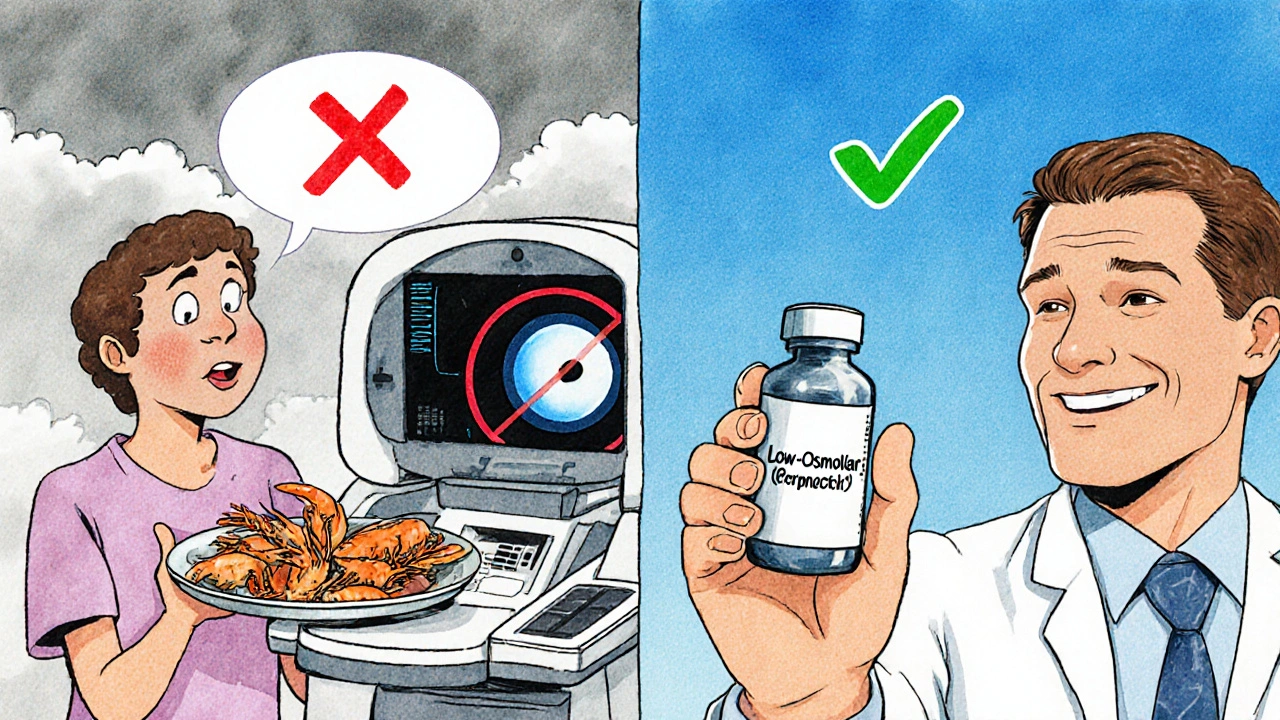
Not everyone does. The American College of Radiology (ACR) says you only need it if you’ve had a prior moderate or severe reaction to iodinated contrast. That’s it. A lot of people think shellfish allergies, iodine allergies, or even Betadine skin prep reactions mean you’re at higher risk. They’re wrong.Studies show people with shellfish allergies have only a 2 to 3 times higher chance of reacting to contrast dye than someone with no history at all. That’s still a tiny risk-less than 1%. No pre-med needed. Same goes for iodine or Betadine. Those aren’t linked to contrast reactions. If your doctor says otherwise, ask for the evidence.
The only real red flag? A previous reaction to the same type of contrast dye. If you reacted to one brand or formulation, you’re more likely to react to another one in the same class. That’s why switching to a different contrast agent-even if it’s still iodinated-is often the first-line recommendation. It’s safer than drugs, cheaper, and just as effective.
The Two Main Premedication Protocols
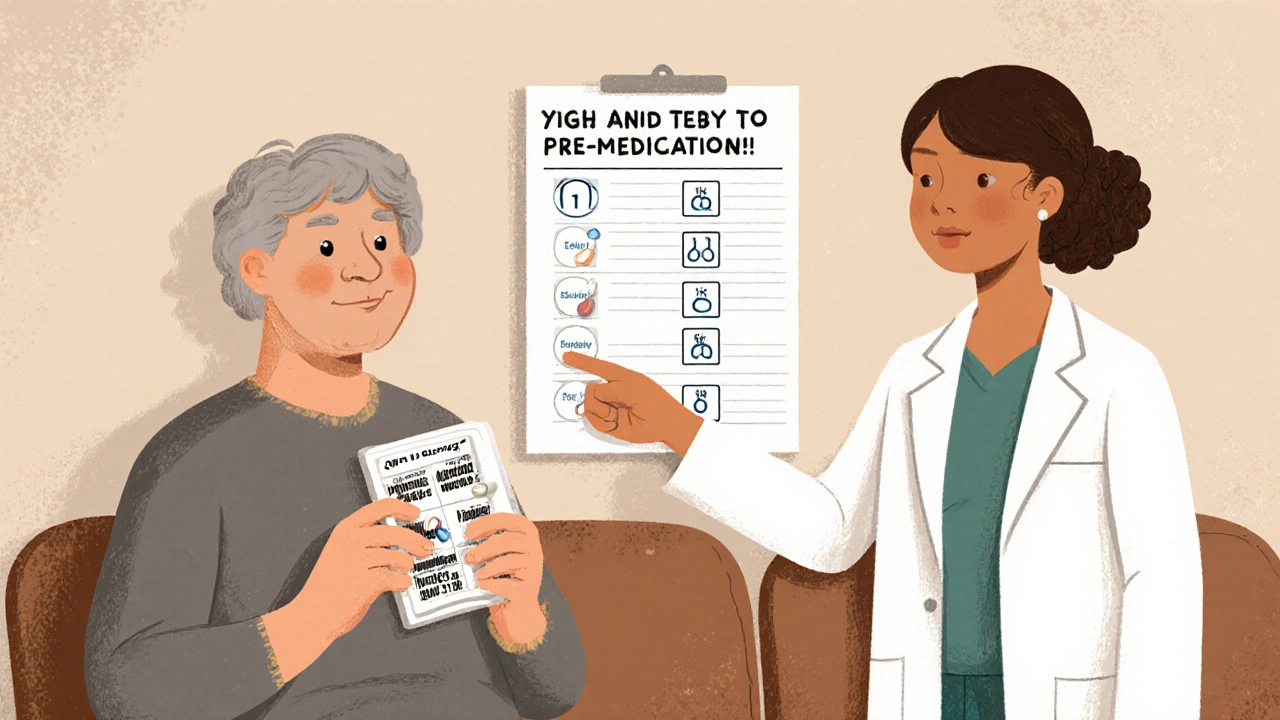
If you need pre-medication, you’ll get a combo of steroids and antihistamines. The goal? Block the body’s inflammatory response before the dye hits your bloodstream.There are two main ways to give it: oral (pill form) and IV (through a vein). Which one you get depends on whether you’re scheduled for a routine scan or an emergency.
Oral Protocol (For Elective Scans)
This is the standard for outpatient imaging. You take pills at home, starting 13 hours before your scan:- Prednisone 50 mg at 13 hours before
- Prednisone 50 mg at 7 hours before
- Prednisone 50 mg at 1 hour before
- Diphenhydramine (Benadryl) 50 mg at 1 hour before
Why so early? Studies show premedication doesn’t work if you start less than 4 to 5 hours before. The steroids need time to quiet your immune system. Benadryl kicks in fast, but it makes you sleepy. That’s why you need someone to drive you home. No exceptions. If you show up alone, they’ll reschedule you.
IV Protocol (For Emergencies or Inpatients)
If you’re in the hospital or the scan can’t wait, you get the drugs through an IV. Two common options:- Methylprednisolone (Solu-Medrol): 40 mg IV, then repeated every 4 hours until just before the scan. Plus 50 mg IV Benadryl 1 hour before.
- Hydrocortisone (Solu-Cortef): 200 mg IV, then repeated every 4 hours until just before the scan. Plus 50 mg IV Benadryl 1 hour before.
These work faster. But they still need at least 4 hours to be effective. If you’re rushed in at 3 a.m. and the team tries to give you a 1-hour IV premed, it won’t help. They’ll have to delay the scan-or skip premed and accept the risk.

What About Kids?
Children under 6 usually don’t get premedication unless they’ve had a severe reaction. For kids 6 and older, if antihistamines alone are enough (no steroids), UCSF recommends cetirizine (Zyrtec) 10 mg by mouth 1 hour before the scan. It’s less sedating than Benadryl, so kids can go to school afterward. Always check with the radiology team-pediatric dosing isn’t just a scaled-down adult dose.What If You’re Still Worried?
Even with pre-medication, about 2% of people still have a reaction. That’s called a “breakthrough” reaction. It’s rare, but it happens. That’s why safety planning isn’t just about taking pills-it’s about where and how the scan is done.- Facilities must have trained staff and crash carts ready within seconds. No exceptions.
- Patients with a history of severe reactions should only be scanned at hospitals with rapid access to ICU-level care-like major academic centers.
- For emergencies, a doctor should accompany the patient to the imaging suite. That way, if something goes wrong, help is right there.
And don’t forget documentation. If you’ve had a reaction before, your referring doctor must consult with a radiologist before scheduling. Some places, like UCLA, even specify which buildings are approved for high-risk patients. This isn’t bureaucracy-it’s a safety net.
Cost and Accessibility
The cost of premedication? Almost nothing. Prednisone pills cost about 25 cents each. Benadryl is 15 cents a dose. That’s less than 0.1% of a typical $1,000 CT scan. Yet, only 78% of community hospitals follow the full protocol. Academic centers? Nearly 100%. Why? Because they’re used to handling high-risk cases. If you’re getting scanned at a small clinic, ask if they’ve done this before. If they hesitate, push for a transfer.The Future of Contrast Safety
Newer contrast dyes are much safer than the old ones. In the 1980s, high-osmolar dyes caused reactions in up to 10% of patients. Today’s low-osmolar dyes? Less than 0.2%. That’s why some experts now question whether we still need premedication for everyone with a prior reaction.Dr. James McDonald’s 2021 study showed that switching to a different contrast agent-even without steroids-can reduce recurrence rates just as much. That’s a game-changer. The ACR is expected to release its next manual in late 2024, and early drafts suggest a stronger push toward agent switching over routine premedication.
For now, the protocols are still standard. But the message is clear: don’t just default to pills. Ask if you can switch the dye first. It’s simpler, cheaper, and just as safe.
What to Do Before Your Scan
If you’ve been told you need pre-medication, here’s your checklist:- Confirm you’ve had a moderate or severe reaction before. If it was mild, you probably don’t need it.
- Ask if you can switch to a different contrast agent. If yes, do that first.
- If premed is still needed, get the exact schedule from the radiology department. Don’t guess.
- Plan for transportation. Benadryl will make you drowsy. No rides? No scan.
- Bring your medication list. Tell them about any other drugs you take.
- Ask where the scan will be done. If it’s not at a hospital with emergency support, push back.
Contrast dye saves lives. But only if it’s used safely. You’re not being paranoid if you ask questions. You’re being smart.
Do shellfish allergies mean I can't have contrast dye?
No. Shellfish allergies have no direct link to contrast dye reactions. Studies show people with shellfish allergies are only 2 to 3 times more likely to react than the general population-which still means less than a 1% risk. Premedication isn’t needed just because you’re allergic to shrimp or crab.
Can I take Benadryl the night before my CT scan?
No. Benadryl needs to be taken 1 hour before the scan to be effective. Taking it the night before won’t help. The steroid part of premedication (like prednisone) needs to be taken 13, 7, and 1 hour before to work properly. Timing matters.
Is it safe to drive after taking Benadryl for contrast dye?
No. Benadryl causes drowsiness, slowed reaction times, and blurred vision. Even if you feel fine, your driving ability is impaired. You must have someone drive you home after your scan. If you don’t, the facility will reschedule your appointment.
What if I miss a dose of my premedication?
If you miss the prednisone doses, especially the last one 1 hour before, your risk of a reaction goes back up. Call the radiology department immediately. They may reschedule or switch to an IV regimen if possible. Never skip the steroid part-it’s the key to reducing recurrence.
Can I get premedication at my local clinic?
Maybe. But only if they have trained staff, emergency equipment, and protocols for managing severe reactions. Many community clinics don’t. If you have a history of a moderate or severe reaction, ask if the scan can be done at a hospital with immediate access to an ICU or emergency team. Safety isn’t optional.



Chris Ashley, November 13, 2025
Bro, I had a CT last year and they tried to make me take Benadryl the night before. I told them nope, read the damn article. They were like ‘uhhh we’ve always done it that way’ - I literally showed them the post on my phone. They rescheduled. Worth it.
kshitij pandey, November 14, 2025
Hey everyone! I'm from India and we don't have this kind of detailed protocol in small hospitals here. But I'm glad someone shared this. My cousin had a reaction once, and they didn't even know what to do. Let's spread awareness - safety is for everyone, no matter where you live!
Brittany C, November 16, 2025
It's fascinating how the ACR guidelines have evolved. The shift from premedication dependency to contrast agent switching reflects a deeper understanding of anaphylactoid mechanisms. The pharmacokinetic window for steroid efficacy is well-documented - 4–5 hours is non-negotiable for FcγR modulation. Still, I'm surprised more institutions don't use low-osmolar non-ionic agents as first-line for high-risk patients.
Sean Evans, November 18, 2025
OMG I can't believe people still think shellfish = contrast allergy 😭 This is why medicine is broken. My cousin got denied a CT because she ate shrimp in 2018. She cried. I cried. We all cried. And now she has a kidney stone and can't get scanned. This isn't medicine - it's superstition with a stethoscope. 🤦♂️
Anjan Patel, November 18, 2025
AND THEN - and then - some people think they can just skip the prednisone because they 'feel fine'?!?!? Are you kidding me?!? I had a friend who did that. She got wheezing in the scanner. They had to call a code blue. She spent three days in ICU. Her mom cried on TikTok. And now she's suing the hospital. THIS ISN'T A GAME. PEOPLE DIE BECAUSE OF THIS. YOU THINK YOU'RE SMART? YOU'RE NOT. YOU'RE A TIKTOK TROLL WITH A CT SCAN.
Scarlett Walker, November 20, 2025
This post literally saved me. I was so scared to get my scan - I thought I’d die. But reading this made me feel like I actually had control. I switched the dye, took my pills on time, and had my boyfriend drive me. No drama. No panic. Just calm, smart prep. You guys are the real MVPs for sharing this.
Hrudananda Rath, November 21, 2025
It is, indeed, a matter of profound regret that the medical establishment continues to adhere to protocols of dubious provenance, despite the overwhelming evidence favoring agent substitution. The reliance upon pharmacological prophylaxis - an antiquated paradigm rooted in the pre-2000s era of high-osmolar contrast media - represents a systemic failure of evidence-based practice. One must question the institutional inertia that permits such suboptimal care to persist.
Brian Bell, November 23, 2025
Just got my CT today - switched dye, took Benadryl at 1 hour, no issues. Felt like a superhero. 😎 Pro tip: Bring snacks. The waiting room is a wasteland. And yes, I had someone drive me. No questions asked.
Nathan Hsu, November 24, 2025
It is critical to note, however, that the ACR guidelines, while authoritative, are not universally adopted - particularly in rural, under-resourced settings - and this disparity constitutes a significant public health inequity. Moreover, the cost-effectiveness argument, while compelling, must be contextualized within the broader framework of healthcare accessibility, wherein socioeconomic status often dictates whether one receives the 'gold standard' of care.
Ashley Durance, November 24, 2025
Most people who post about this clearly haven’t read the full ACR manual. The 2023 update clarified that mild reactions don’t qualify for premedication - yet 90% of the comments here are still confused. You’re not ‘being safe’ - you’re being misinformed. Also, Benadryl at night? That’s not just wrong - it’s dangerous. Stop.
Scott Saleska, November 24, 2025
So… I had a reaction once, like 8 years ago. Mild rash. I didn’t tell anyone. Now I’m getting a scan next week. Should I say something? I mean… I don’t want to make a big deal. But also… I don’t want to die. What do I do?
Ryan Anderson, November 26, 2025
You absolutely tell them. Even if it was mild. Even if it was years ago. They’ll ask you for details - date, symptoms, treatment. Write it down. Bring it. This isn’t being dramatic - it’s your body’s history. And if they hesitate? Say, ‘I’ve read the ACR guidelines. I’m not asking for a favor. I’m asking for safety.’ You’re not being difficult. You’re being responsible.
Eleanora Keene, November 26, 2025
Thank you for this! I'm a nurse and I've seen so many patients scared to speak up. This is the kind of info that empowers people. I always tell my patients: 'You are your own best advocate.' Don't let anyone make you feel silly for asking questions - especially when your life is on the line. And yes, if you need a ride - get one. No shame.
Joe Goodrow, November 26, 2025
Why are we letting some fancy doctor from UCLA tell us how to do medicine? In America, we don’t need all this extra crap. My uncle got contrast in ’92 - no premed, no problems. We’re getting soft. Just take the scan. Stop overthinking. This is why healthcare costs are so high - because of people like you who turn every scan into a TED Talk.