Every year, thousands of children are put at risk because a dose of medicine was calculated wrong. Not because a pharmacist was careless. Not because a doctor made a sloppy mistake. But because a weight was entered in pounds instead of kilograms. Or because the last weight recorded was from six months ago. Or because the system didn’t stop the order when the dose was five times too high. These aren’t hypotheticals. They’re real, preventable errors-and they happen more often than most people realize.
Why Weight Matters More Than Anything Else in Pediatric Dosing
Adults get doses based on fixed amounts: one tablet, 10 mL, 500 mg. Kids don’t. Their bodies are smaller, their organs are still developing, and their metabolism changes fast. That’s why pediatric dosing is almost always calculated by weight: milligrams per kilogram (mg/kg). A 5 kg baby needs a completely different dose than a 40 kg child, even if they’re both diagnosed with the same infection.
But here’s the problem: humans are bad at math under pressure. A nurse rushing to get a child settled before surgery. A pharmacist juggling ten prescriptions at once. A doctor typing fast in an EHR system. All of them can miss a decimal point. Or confuse pounds with kilograms. Or assume the weight on the chart is still accurate.
According to the World Health Organization, children are three times more likely to suffer a medication error than adults. And nearly 20% of those errors come down to weight miscalculations. That’s not a small risk. That’s a systemic flaw.
The Three Critical Points Where Errors Happen
Preventing these errors isn’t about one magic fix. It’s about building layers of defense-at three key moments:
- Prescription entry: When the doctor types the order.
- Pharmacy verification: When the pharmacist checks and dispenses it.
- Bedside administration: When the nurse gives the drug to the child.
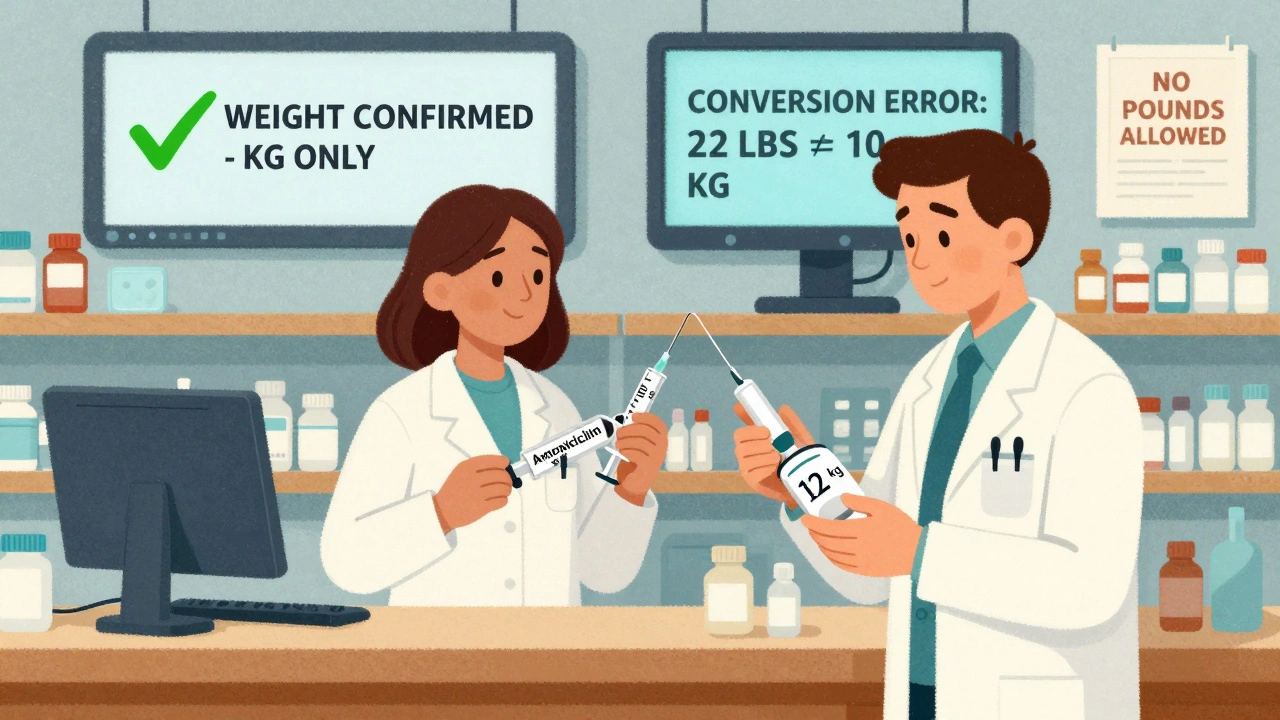
At each point, weight must be verified-not just checked, but confirmed. And it must be in kilograms. Always. No exceptions.
Why kilograms? Because every major guideline-from the American Society of Health-System Pharmacists to the American Academy of Pediatrics-mandates it. Pounds are a source of error. Converting 22 pounds to 10 kg? Easy. But 22.5 pounds to 10.2 kg? That’s where mistakes creep in. A 2022 study found that 12.6% of pediatric dosing errors were caused by pounds-to-kilograms conversions alone. Eliminate the conversion, and you eliminate that whole category of error.
What a Real Weight-Based Verification System Looks Like
It’s not just about having a weight field in the computer. It’s about forcing the system to work for safety.
First, the EHR must require weight entry before any pediatric prescription can be submitted. No weight? No order. Period. That’s not optional. It’s the baseline.
Second, the system must include clinical decision support (CDSS) that flags dangerous doses. If a child weighs 12 kg and the order is for 150 mg of amoxicillin, the system should know that’s way above the safe upper limit. It should stop the order and ask: “Are you sure?” Not just a pop-up. A hard stop.
Third, the pharmacy must have a mandatory dual verification step. One pharmacist calculates. A second pharmacist rechecks. No shortcuts. This isn’t bureaucracy-it’s a safety net. A 2021 review showed that pharmacist-led verification reduced administration errors by 15.8 percentage points. That’s not a minor gain. That’s life-saving.
And at the bedside? Barcode scanning must include weight data. If the system knows the child weighs 18 kg and the label says “10 mL of 25 mg/mL vancomycin,” it should cross-check that against the prescribed dose. If it doesn’t match? The scan fails. The medication doesn’t go in.
Technology Isn’t Enough-But It’s Necessary
Some hospitals still use paper charts and handwritten orders. They rely on staff memory and manual calculations. Those places have error rates three to five times higher than hospitals with full electronic systems.
A 2022 study in the Journal of the American Medical Informatics Association found that when EHRs had properly configured weight-based alerts, dosing errors dropped by 87.3%. That’s not a slight improvement. That’s a revolution.
But tech can backfire. Alert fatigue is real. If the system flags every single dose as “potentially high,” clinicians start ignoring it. A 2021 study found that 41.7% of weight-based alerts were overridden-and 18.3% of those overrides were actual errors that should’ve been caught.
The fix? Smarter alerts. Epic Systems’ 2024 Pediatric Safety Module 4.0 uses growth percentiles instead of fixed weight limits. If a 10-year-old weighs 30 kg, but their growth curve shows they’ve been steady at 28 kg for a year, the system won’t flag a 10% dose increase as dangerous. It learns. It adapts. It reduces false alarms by 63%.
What Happens When You Don’t Get This Right
One nurse in a rural hospital forgot to update a child’s weight after a hospital stay. The child weighed 16 kg, but the chart still said 12 kg. The prescribed dose of ceftriaxone was calculated for 12 kg. The child got 33% more than they should have. They developed seizures. They spent three days in the PICU.
That wasn’t malice. It wasn’t incompetence. It was a broken process.
Another case: a community pharmacy didn’t have access to the child’s EHR. The parent brought in a prescription. The weight on the slip was handwritten: “30 lbs.” The pharmacist converted it to 13.6 kg. But the child actually weighed 15 kg. The dose was too low. The infection didn’t clear. The child came back two weeks later with pneumonia.
These aren’t rare. A 2022 survey of 1,247 pediatric nurses found that 63.2% had seen weight documentation errors in the past year. And 41.7% said those errors caused medication delays-meaning kids waited longer for treatment because staff had to stop, recheck, and re-calculate.
How to Build a Reliable System-Step by Step
It’s not about spending millions. It’s about doing the basics right.
- Standardize units: All weights must be entered and displayed in kilograms. No pounds. No ounces. No “approximate.” Digital scales in pediatric units must show only kilograms, to 0.1 kg for infants, 0.5 kg for older kids.
- Require weight on every order: No weight = no prescription. The EHR must block submission until weight is entered and confirmed.
- Use standardized concentrations: Don’t let every drug come in different strengths. Standardize vancomycin to 5 mg/mL, amoxicillin to 250 mg/5 mL. Fewer calculations = fewer errors.
- Implement dual verification: One pharmacist calculates. A second verifies. Both sign off. No exceptions.
- Update weight regularly: Weight must be measured within 24 hours for inpatients. For outpatients, it must be updated every 30 days. Outdated weights are the silent killer.
- Train everyone: Nurses, doctors, pharmacists, even receptionists who weigh kids. Forty hours of training per person isn’t excessive-it’s essential.
Facilities that did this saw weight-related errors drop by over 90% within 18 months. Boston Children’s Hospital cut their conversion errors from 14.3 per 10,000 doses to just 0.8. That’s not luck. That’s discipline.

The Hidden Gap: Rural and Under-Resourced Hospitals
Here’s the uncomfortable truth: the best systems are in big children’s hospitals. Academic centers. Urban teaching hospitals. They have the staff. The tech. The funding.
But only 32.7% of rural community hospitals have full weight-based verification systems. That means kids in small towns, in low-income areas, are at higher risk-not because their families are careless, but because the system failed them.
That’s not just a healthcare gap. It’s a justice gap.
There are low-cost solutions: printed weight-based dosing charts. Simple checklists. Mandatory phone calls to the prescribing clinic if weight is missing. These aren’t glamorous. But they save lives.
The Future: AI, Wearables, and a Culture of Safety
The next wave is smarter tech. AI that predicts a child’s expected weight based on age, height, and past records. Wearables that track weight changes in kids with chronic conditions. Blockchain to lock weight data so it can’t be altered.
But the most important tool isn’t tech. It’s culture.
Dr. Robert Wachter from UCSF says it plainly: “Technology alone cannot prevent errors. A culture of safety with non-punitive error reporting is essential.”
That means if a nurse spots a wrong weight and speaks up, they’re thanked-not punished. If a pharmacist catches a bad dose, they’re celebrated. If a system fails, you fix the system, not the person.
Because the goal isn’t perfection. It’s protection. Every child deserves a dose that’s calculated right. Not because someone remembered. But because the system made sure.
What You Can Do Today
Whether you’re a pharmacist, a nurse, a parent, or a hospital administrator, here’s what matters now:
- If you’re in a clinical setting: Ask for the child’s most recent weight. Don’t assume. Don’t guess.
- If you’re a parent: Know your child’s weight in kilograms. Bring it with you. Write it down. Say it out loud.
- If you’re in leadership: Require weight-based verification. Don’t wait for a tragedy to act.
Medication errors in children aren’t inevitable. They’re preventable. And the tool to stop them? It’s not expensive. It’s not complicated. It’s just a number. And the unit it’s measured in.




Gene Linetsky, December 4, 2025
They still use pounds in some hospitals? That’s not negligence, that’s a death sentence waiting to happen. I’ve seen nurses convert 30 lbs to 15 kg and call it good. No wonder kids end up in PICU.
Archie singh, December 6, 2025
Let’s be clear-this isn’t about tech. It’s about accountability. Hospitals that skip dual verification are playing Russian roulette with pediatric lives. The fact that this even needs explaining is a national disgrace. No more ‘oops’-only consequences.
Jim Schultz, December 6, 2025
Look, I get it-weight-based dosing is critical. But let’s not pretend that EHRs are magic. I’ve worked in three hospitals where the system flagged every dose as ‘dangerous’ because someone entered 12.5 kg instead of 12.4. Clinicians stopped trusting it. Then the real errors slipped through. It’s not the system’s fault-it’s the lazy config. Fix the alerts, not the people.
And don’t even get me started on ‘standardized concentrations.’ If you think every hospital can afford to re-stock every drug in 5mg/mL increments, you’ve never seen a rural pharmacy’s budget. Real-world constraints exist. Stop pretending this is a software bug.
Also, ‘block submission until weight is entered’? Great. What if the scale is broken? What if the kid’s in the ER and they’re screaming and the mom doesn’t know the weight? You’re not fixing a problem-you’re creating a bottleneck that delays care. And that kills too.
Yes, conversion errors are bad. Yes, outdated weights are dangerous. But your solution reads like a PowerPoint slide from a consultant who’s never held a crying toddler in their arms while a nurse scrambles to find a scale. You’re diagnosing the disease but prescribing the wrong medicine.
And before you say ‘well, that’s why we need training’-yes, we do. But training doesn’t fix broken systems. It just makes people better at working around them. That’s not safety. That’s adaptation. And adaptation is how you get 41.7% of alerts overridden.
So yes, I agree with the goal. But your method? It’s arrogant. It’s unrealistic. And frankly, it’s insulting to the frontline workers who are trying to do their jobs under impossible conditions.
Ignacio Pacheco, December 7, 2025
So we’re blaming the conversion from pounds to kilograms, but not the fact that most pediatric scales in the U.S. default to pounds? That’s like blaming drivers for running red lights because the traffic signal was red when it should’ve been green. The system’s designed to fail. Why are we still surprised?
And the ‘AI predicts weight based on height and past records’ bit? Cute. What if the kid’s had a growth spurt? Or a recent illness? Or they’re a preemie who’s catching up? AI doesn’t know that. Only the parent or the nurse does. So now we’re automating ignorance?
Also-‘block submission until weight is entered’-great. But what if the child’s weight is unknown? Like, say, a newborn in the NICU? Do we just refuse to treat them until we weigh them? That’s not safety. That’s protocol theater.
And the ‘dual verification’ requirement? Sounds great until you’re the only pharmacist on shift at 3 a.m. and you’ve got five kids on antibiotics, two overdoses, and a code blue down the hall. Now you’re supposed to wait for a second pharmacist who’s asleep? That’s not a safety net. That’s a liability.
Bottom line: the problem isn’t the unit. It’s the culture of rushing, understaffing, and pretending tech can fix human systems. Fix the staffing. Fix the burnout. Then the weights will get entered right.
Chloe Madison, December 8, 2025
I work in a pediatric clinic in rural Ohio. We don’t have an EHR. We use paper forms. We don’t have dual verification. But we do have a laminated card taped to every scale: ‘WEIGHT IN KG ONLY.’ Every nurse, every PA, every front desk person knows it. We write it in red ink. We say it out loud: ‘Weight is 14.5 kg.’ We confirm it with the parent. We don’t assume. We don’t guess. And we’ve had zero weight-related errors in three years.
It’s not about the tech. It’s about the habit. The ritual. The discipline. You don’t need AI to save a child’s life-you just need someone who refuses to cut corners.
And if you’re a parent? Bring the weight. Write it on your hand. Say it three times. Your kid’s life depends on it. Don’t wait for the system to save you-be the safety net.
Makenzie Keely, December 9, 2025
Let’s talk about the real crisis: rural hospitals. 32.7% have full systems? That means nearly 70% of kids in small-town America are being dosed on guesswork. That’s not a healthcare disparity-that’s a civil rights violation. These aren’t just stats-they’re children. And they’re dying because their zip code determines whether they get a safe dose.
And yet, no one’s funding the low-cost fixes: printed charts, checklist posters, mandatory phone calls to the prescribing clinic. Why? Because it’s not sexy. It doesn’t look good in a grant proposal. But it saves lives.
My sister works in a clinic that uses a simple laminated chart with weight ranges and corresponding doses. No computer. No alerts. Just a piece of paper. And they’ve cut their errors by 89%. So why aren’t we scaling this? Why are we pouring millions into AI when a $20 laminated sheet does the job?
It’s not about technology. It’s about priorities. And right now, we’re prioritizing innovation over survival.
Kidar Saleh, December 10, 2025
As someone who trained in the NHS and now works in U.S. pediatrics, I’ve seen both systems. The UK uses kilograms exclusively-no exceptions. No conversions. No debates. It’s built into the culture. And you know what? Errors are lower. Not because British nurses are smarter-but because the system doesn’t let them fail.
Here’s the truth: American medicine treats safety like an optional add-on. In Europe? It’s the foundation. We don’t need more tech. We need a cultural reset. Stop treating pediatric dosing like a math quiz and start treating it like a sacred duty.
And parents? Don’t be afraid to say: ‘My child weighs 16.3 kg.’ Say it like it’s a fact. Because it is. And if they hesitate? Push back. Your silence is their risk.
Vincent Soldja, December 11, 2025
Agreed.