Rifampin Drug Interaction Checker
Medication Interaction Check
Check for dangerous interactions between rifampin and your current medications. This tool identifies high-risk combinations based on the latest clinical evidence.
Rifampin Timing Calculator
Calculate when it's safe to restart other medications after stopping rifampin.
Wait 4 weeks after stopping rifampin
Wait 2 weeks after stopping rifampin
When treating tuberculosis, rifampin is one of the most powerful drugs doctors have. It cuts treatment time from 18 months to just six. But here’s the catch: rifampin doesn’t just kill TB bacteria-it also changes how your body handles almost every other medication you take. This isn’t a minor side effect. It’s a major clinical challenge that can lead to treatment failure, dangerous side effects, or even death if not managed properly.
How Rifampin Actually Works
Rifampin, also called rifampicin, is a semi-synthetic antibiotic that targets the RNA polymerase enzyme in Mycobacterium tuberculosis. By binding to the beta-subunit of this enzyme, it shuts down bacterial RNA production. Without RNA, the bacteria can’t make proteins or replicate. It’s fast, effective, and kills both active and dormant TB bugs inside and outside human cells.
A single 600 mg oral dose raises blood levels to an average of 7 mcg/mL within a few hours. But eat food with it? Absorption drops by 30%. That’s why it’s always taken on an empty stomach-usually one hour before breakfast. This precision matters because even small drops in concentration can let some bacteria survive and develop resistance.
The Hidden Power: Enzyme Induction
Rifampin’s real superpower-and its biggest danger-is how it turns on your body’s drug-processing system. It activates a nuclear receptor called PXR. This receptor acts like a master switch, flipping on genes that produce CYP3A4, UDP-glucuronosyltransferases, and P-glycoprotein. These are the enzymes and transporters that break down and clear drugs from your blood.
Within 24 hours of taking rifampin, your liver starts making more CYP3A4. By day three, enzyme activity spikes by 200-400%. After five to seven days, it hits peak induction. And here’s the kicker: even after you stop rifampin, these enzymes stick around for up to two weeks. That means any drug you take during or shortly after rifampin therapy could be broken down too fast to work.
Life-Threatening Interactions
Here’s where things get dangerous. Rifampin doesn’t just affect one or two drugs-it affects dozens. The most common and serious interactions include:
- Oral contraceptives: Rifampin cuts hormone levels by up to 67%. Women on birth control pills can become pregnant even if they take them perfectly. No backup method? That’s a real risk.
- Warfarin: This blood thinner’s effectiveness drops by 42%. Patients on warfarin need frequent INR checks. A missed adjustment can lead to clots or dangerous bleeding.
- HIV protease inhibitors: Drugs like lopinavir and atazanavir lose 75-90% of their concentration. This isn’t just a treatment failure-it’s a gateway to drug-resistant HIV.
- Antifungals, statins, immunosuppressants: All are weakened. Tacrolimus levels can crash in transplant patients. Simvastatin can become ineffective, raising heart disease risk.
Doctors often miss these interactions because patients don’t list all their medications. A woman on birth control might not mention it. An older adult might not realize their cholesterol pill is now useless. The result? Unintended consequences that could have been avoided.
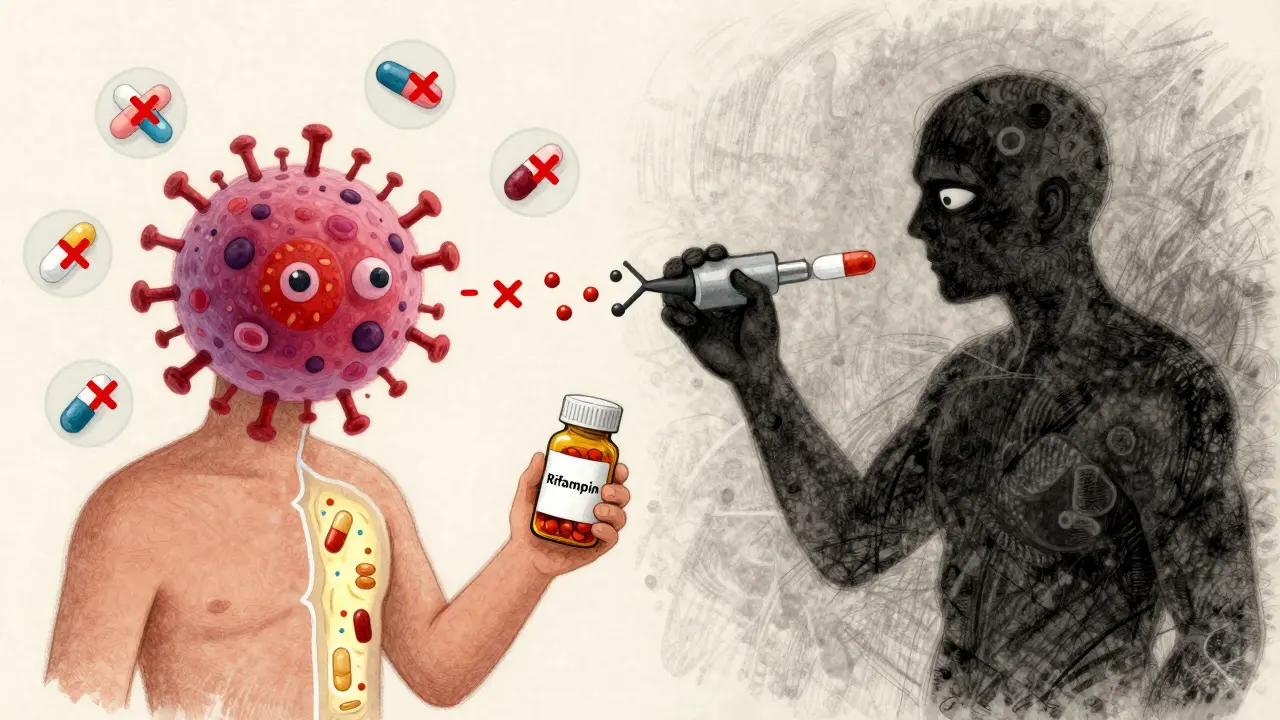
The Paradox: Rifampin Creates Its Own Enemy
Here’s something even more surprising: rifampin doesn’t just interact with other drugs-it helps TB bacteria survive it.
Research shows that within hours of exposure to rifampin, a small group of TB bacteria starts pumping the drug out using efflux pumps. These are like tiny bouncers at the cell door, kicking rifampin back out before it can kill. Even worse, rifampin itself triggers the bacteria to produce more of a protein called RpoB, which helps them tolerate the drug. This isn’t genetic resistance-it’s a temporary survival tactic that kicks in within 3 hours.
This self-induced tolerance explains why TB treatment takes so long. Even if 99% of the bacteria die, that 1% can bounce back. That’s why six months of combination therapy is non-negotiable. Shorter courses? Relapse rates jump above 25%.
New Hope: Blocking the Escape Routes
But there’s a promising twist. Scientists found that some common drugs can block those bacterial efflux pumps. Verapamil, a heart medication, and omeprazole, a stomach acid reducer, both stop TB from kicking rifampin out of its cells.
In lab studies, omeprazole at normal clinical doses blocked 68% of rifampin efflux. Verapamil did the same. When added to TB treatment in mice, these drugs cut relapse rates from 25% to under 5%. That’s huge. If this works in humans, we could shorten treatment from six months to three-without losing effectiveness.
What’s even better? Both drugs are already approved, widely available, and have known safety profiles. Repurposing them could be faster and cheaper than developing new antibiotics. Clinical trials are now testing this combo in humans.

Managing Rifampin in Real Life
If you’re on rifampin, here’s what you need to do:
- Tell every doctor you see. Even your dentist or dermatologist. Rifampin changes how every drug works.
- Don’t start or stop other meds without checking. This includes over-the-counter herbs, supplements, and painkillers. St. John’s wort? It’s another CYP3A4 inducer. Combine it with rifampin? Double the risk.
- Use non-hormonal birth control. Condoms, IUDs, or implants. Pills, patches, and rings won’t cut it.
- Monitor liver function. Rifampin can cause liver injury in 10-20% of patients. Watch for yellow skin, dark urine, or unexplained fatigue. Get ALT levels checked monthly.
- Wait two weeks after stopping rifampin before starting sensitive drugs. For warfarin, immunosuppressants, or HIV meds, wait four weeks. The enzymes don’t vanish overnight.
And if you’re a healthcare provider? Always run a drug interaction check before prescribing. Don’t assume the patient knows what they’re taking. Use tools like Lexicomp or Micromedex. A quick lookup could save a life.
Why This Matters Globally
Every year, 3.5 million people start TB treatment with rifampin. It’s the backbone of global TB control. But if we ignore its interactions, we’re setting up patients for failure. Drug-resistant TB is rising. Relapses are costly. Deaths are preventable.
The science is clear: rifampin is indispensable. But it’s not simple. It’s a precision tool that demands precision use. Understanding its induction power isn’t just academic-it’s the difference between curing TB and watching it come back.
Future treatments may include higher rifampin doses (up to 900 mg daily) or adding verapamil or omeprazole. But until those are standard, the best defense is awareness. Know the interactions. Check the list. Ask the questions. Because when rifampin is involved, nothing else works the same way.
Can I take birth control pills while on rifampin?
No. Rifampin reduces hormone levels in birth control pills, patches, and rings by up to 67%, making them unreliable. Use non-hormonal methods like condoms, copper IUDs, or implants instead. Even perfect pill use won’t prevent pregnancy if you’re on rifampin.
How long does rifampin’s effect last after I stop taking it?
The enzyme induction caused by rifampin can persist for up to two weeks after you stop taking it. For drugs with narrow therapeutic windows-like warfarin, tacrolimus, or HIV medications-you should wait four weeks before starting them to ensure enzyme levels return to normal.
Can I take omeprazole or verapamil with rifampin for TB?
Currently, this is not standard practice, but research shows it works in lab and animal models. Omeprazole and verapamil block bacterial efflux pumps that make TB resistant to rifampin. Clinical trials are underway to test whether adding these drugs can shorten TB treatment from six months to three. Talk to your doctor if you’re interested in participating.
Why does rifampin cause liver damage?
Rifampin can cause drug-induced liver injury by triggering oxidative stress, damaging mitochondria, and altering liver enzyme activity. About 10-20% of patients on TB treatment show ALT levels more than three times the upper limit of normal. Regular blood tests are essential. Symptoms like nausea, fatigue, yellow skin, or dark urine need immediate evaluation.
Is rifampin still the best TB drug despite its interactions?
Yes. Rifampin remains the most effective drug for shortening TB treatment from 18 months to six months. No other first-line drug matches its ability to kill both active and dormant TB bacteria. While its interactions are complex, they’re manageable with proper monitoring. For now, it’s still the cornerstone of global TB control.



Amy Ehinger, January 15, 2026
I’ve been on rifampin for six months now, and honestly? The biggest surprise wasn’t the side effects-it was how many people around me were on meds that suddenly stopped working. My grandma’s blood pressure pill? Gone. My friend’s antidepressant? Useless. I started keeping a list of everything I took and gave copies to every doctor I saw. It’s annoying, but it saved me from a hospital trip when my INR went haywire. Just… don’t assume anything. Tell everyone. Even the guy at the pharmacy who doesn’t ask.
RUTH DE OLIVEIRA ALVES, January 16, 2026
It is imperative to underscore the clinical significance of rifampin’s potent induction of hepatic cytochrome P450 enzymes, particularly CYP3A4, which demonstrably alters the pharmacokinetic profiles of concomitantly administered pharmaceutical agents. Failure to account for this phenomenon constitutes a significant breach in therapeutic safety protocols, especially in polypharmacy contexts. Adherence to established guidelines regarding drug interaction screening, non-hormonal contraception, and post-therapy washout periods is not merely advisable-it is ethically obligatory.
Niki Van den Bossche, January 18, 2026
Think about it: rifampin doesn’t just kill bacteria-it reprograms your entire biochemical identity. You’re not just taking a drug; you’re becoming a walking pharmacological paradox. Your liver becomes a factory for drug-disassemblers, your hormones vanish like smoke, and your immune system forgets how to recognize threats. Is this medicine-or is it a silent metamorphosis? We treat TB like a war, but maybe we’re just turning patients into collateral damage in a biochemical arms race we don’t fully understand. And yet… we keep doing it. Because what else is there?
Nilesh Khedekar, January 19, 2026
Wow. So let me get this straight-India has 25% of the world’s TB cases, and we’re still using a drug that makes birth control useless and warfarin useless and HIV meds useless? And you’re telling me the solution is to add omeprazole? That’s a stomach pill. Are we seriously trying to fix a global health crisis with over-the-counter antacids? I’m not impressed. We need real drugs, not kitchen cabinet hacks. And why is this even a surprise? We’ve known about enzyme induction since the 80s.
Crystel Ann, January 21, 2026
This post made me feel seen. I was on rifampin last year and didn’t realize my thyroid med was no longer working until I started crashing. My endocrinologist didn’t even ask about my TB meds. I had to bring the research myself. It’s exhausting being the person who has to explain everything. But I’m glad someone finally wrote this out clearly. Please, if you’re on this drug-speak up. Even if it feels awkward. It’s worth it.
Nat Young, January 22, 2026
Let’s be real-rifampin is just the latest in a long line of drugs that work great until they don’t, and then we blame patients for not reading the fine print. Meanwhile, pharma companies knew this for decades and never bothered to make a safer version. Now they’re slapping on a ‘hey, take this antacid’ bandaid and calling it innovation? Please. If you’re going to use a nuclear option, at least make the nuclear waste safe. Otherwise, stop pretending you’re helping people.
Jan Hess, January 24, 2026
This is actually really cool. I’m a nurse and I’ve seen so many patients get hit by these interactions. But the part about omeprazole and verapamil blocking the efflux pumps? That’s the kind of thing that gives me hope. Repurposing old drugs is genius. Cheaper. Faster. Safer. We need more of this. I’m telling my whole team tomorrow. Maybe we can get a pilot going at our clinic. If we can cut treatment time in half without losing efficacy? That’s a game changer for people who can’t afford six months off work.
Haley Graves, January 24, 2026
If you’re on rifampin, treat it like you’re handling a live grenade. Don’t guess. Don’t assume. Don’t trust your memory. Write it down. Tell every provider. Use a pill organizer with a checklist. Set phone reminders for liver tests. And if you’re a woman of childbearing age? Stop using pills. Period. No exceptions. This isn’t hype-it’s survival. You’re not being paranoid. You’re being smart.
Diane Hendriks, January 24, 2026
Why are we letting foreign pharmaceutical companies dictate how we treat TB? Rifampin was developed in the West, and now we’re stuck with a drug that breaks our own people’s bodies. We need our own TB drugs-developed here, tested here, controlled here. Not some European chemical that makes birth control useless and kills liver enzymes. This isn’t science. It’s colonial medicine.
Sohan Jindal, January 25, 2026
They’re hiding something. Rifampin is too powerful. Too many people get sick after taking it. Why do they keep pushing it? Why not just use something else? And now they want us to take stomach medicine with it? That’s not medicine. That’s a cover-up. I bet they’re doing this so they can sell more drugs later. Big Pharma. Always. Watch your back.
Frank Geurts, January 25, 2026
While the clinical implications of rifampin-induced enzyme induction are undeniably profound, it is equally critical to acknowledge the ethical imperative of patient education and interdisciplinary coordination in mitigating these risks. The integration of pharmacogenomic screening, electronic health record-based drug interaction alerts, and mandatory patient counseling protocols represents not merely a best practice, but a moral obligation in the stewardship of public health. The path forward demands rigor, humility, and systemic accountability.