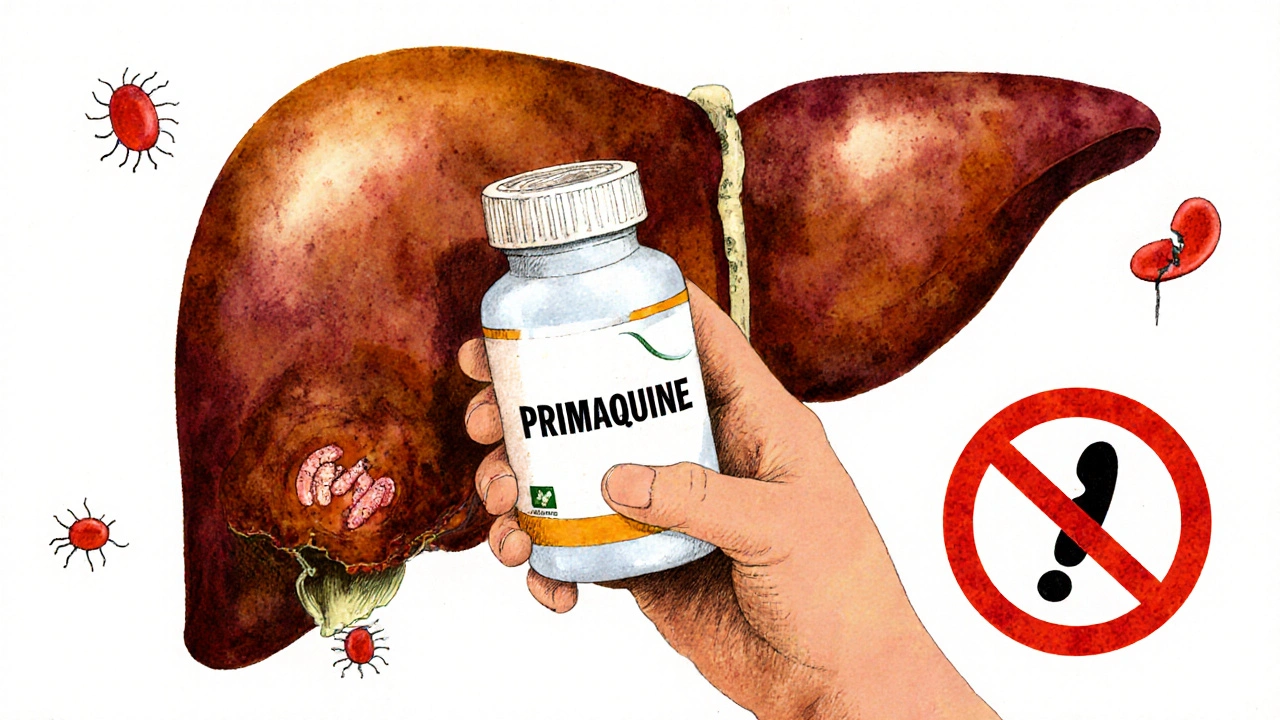
Primaquine is a medication used to prevent malaria relapses, especially in cases caused by Plasmodium vivax and Plasmodium ovale. It’s often prescribed after other antimalarials like chloroquine to kill dormant liver parasites that can wake up weeks or months later. But while it’s effective, it’s not without risks. Many people take it without knowing what could go wrong - and that’s where things get dangerous.
What primaquine does - and why it’s not just another pill
Primaquine works by targeting the dormant forms of malaria parasites hiding in your liver. Unlike other antimalarials that only attack the blood stage, primaquine clears out the hidden reservoirs. That’s why it’s critical for travelers returning from places like Southeast Asia, South America, or parts of Africa where these parasite types are common. But here’s the catch: it only works if your body can process it correctly - and not everyone can.
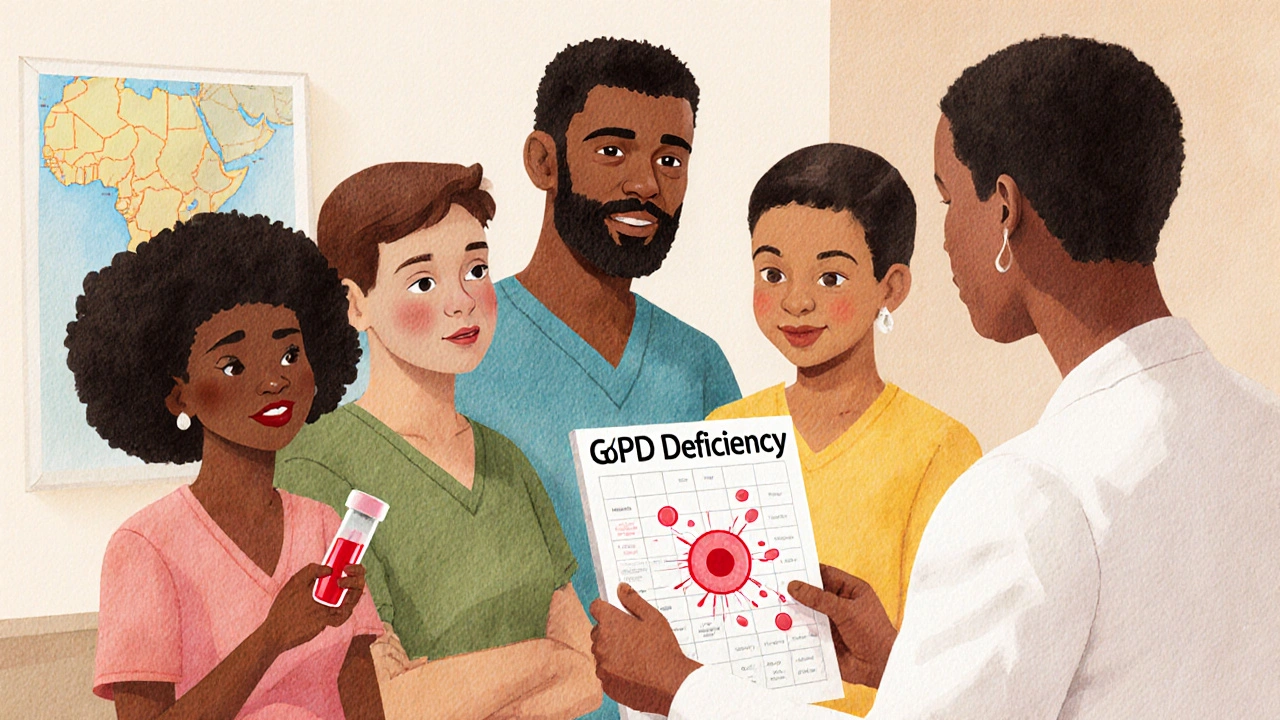
The biggest risk: hemolytic anemia in G6PD-deficient people
The most serious side effect of primaquine is hemolytic anemia - a condition where red blood cells break down too fast. This doesn’t happen to everyone. It only affects people with a genetic condition called glucose-6-phosphate dehydrogenase (G6PD) deficiency. About 400 million people worldwide have this, mostly of African, Mediterranean, or Southeast Asian descent. In the UK, it’s less common but still present, especially among communities with ancestry from those regions.
If you’re G6PD deficient and take primaquine, your red blood cells can’t handle the oxidative stress the drug causes. They burst, leading to fatigue, dark urine, jaundice, and in severe cases, kidney failure or shock. This isn’t a rare reaction - it’s the leading reason primaquine causes hospitalizations. That’s why doctors are supposed to test your G6PD levels before prescribing it. If they don’t, you’re at risk.
Other common side effects you might not expect
Even if you’re not G6PD deficient, primaquine can still cause unpleasant reactions. The most frequent ones include:
- Nausea and vomiting - especially if taken on an empty stomach
- Stomach cramps or bloating
- Dizziness or lightheadedness
- Headaches
- Heartburn or indigestion
These usually show up within the first few days of starting the drug and often fade as your body adjusts. Taking it with food helps reduce stomach upset. But if vomiting is severe or you can’t keep the pill down, contact your provider - you might need a different treatment.
Less common but serious reactions
Some side effects are rare but require immediate attention:
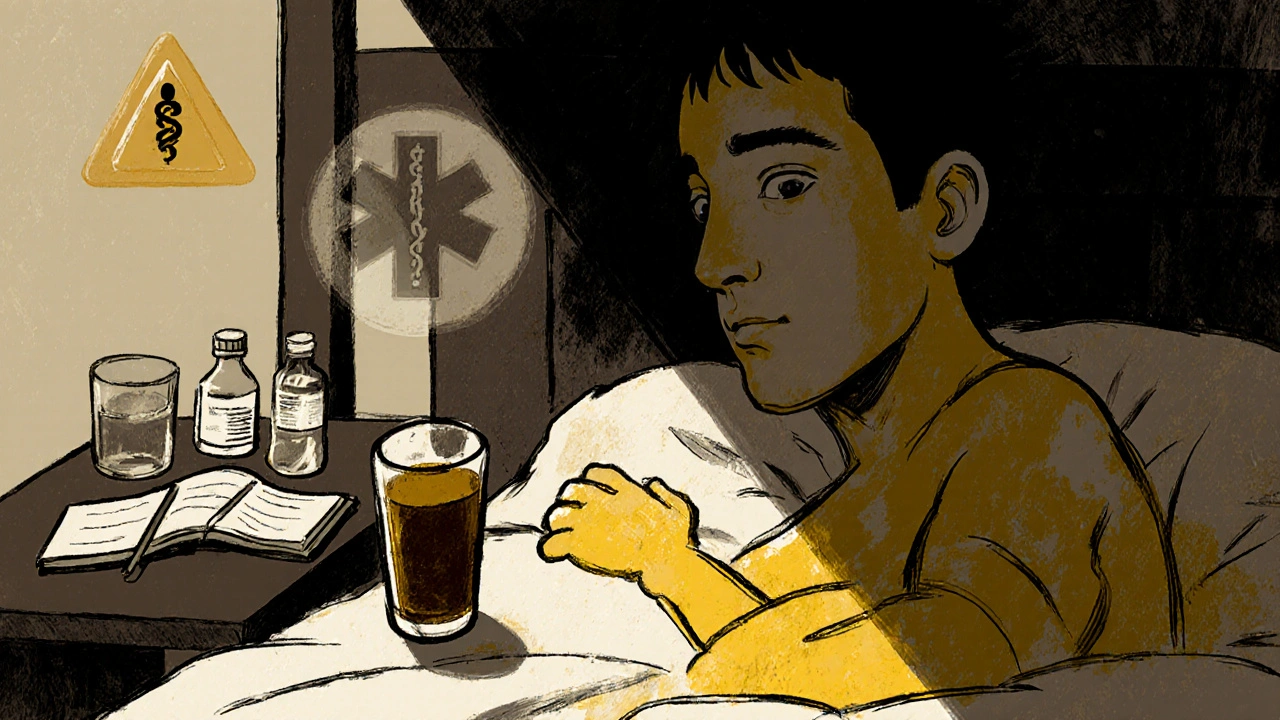
- Dark or tea-colored urine - a sign of red blood cell breakdown
- Yellowing of the skin or eyes (jaundice)
- Unexplained fever or chills
- Rapid heartbeat or shortness of breath
- Severe skin rash or blistering
If you notice any of these, stop taking primaquine and seek medical help right away. These could signal a serious reaction beyond simple side effects. In rare cases, primaquine has been linked to methemoglobinemia - a condition where your blood can’t carry oxygen properly. Symptoms include bluish lips or skin, confusion, and fatigue. It’s more likely in people with certain enzyme disorders or those taking other drugs like sulfonamides or nitrites.
Who should never take primaquine?
Primaquine isn’t safe for everyone. You should avoid it if:
- You’ve been tested and have G6PD deficiency
- You’re pregnant - it can harm the fetus, especially in the first trimester
- You’re breastfeeding and your baby has unknown G6PD status
- You have a history of severe allergic reactions to primaquine or similar drugs
- You have active systemic infections like sepsis or severe liver disease
Even if you’ve taken primaquine before without issues, don’t assume it’s safe every time. Your health can change. A new medication, an infection, or even a change in diet can alter how your body handles the drug.
What to do before and during treatment
Before starting primaquine, make sure your doctor has:
- Ordered a G6PD blood test - don’t rely on family history alone
- Reviewed all your current medications - some interact badly with primaquine
- Asked about your ancestry and past reactions to drugs
During treatment:
- Take the pill with food to reduce nausea
- Drink plenty of water - staying hydrated helps your kidneys flush out byproducts
- Watch for signs of anemia or jaundice - check your urine color daily
- Don’t skip doses - incomplete treatment can lead to drug resistance
Keep a small notebook. Write down any new symptoms, no matter how small. Even mild dizziness or a strange taste in your mouth could be an early warning.
What happens if you miss a dose or take too much?
If you miss a dose, take it as soon as you remember - unless it’s close to your next scheduled dose. Then skip the missed one. Never double up. Taking too much primaquine increases the risk of severe toxicity, especially if you’re undiagnosed with G6PD deficiency.
Overdose symptoms include vomiting, confusion, seizures, and breathing trouble. If you think you’ve taken too much, call emergency services immediately. There’s no antidote, but supportive care - like oxygen, IV fluids, and blood transfusions - can save your life.
How primaquine compares to other radical cure options
Primaquine isn’t the only drug used to prevent relapses. Tafenoquine is a newer alternative that works in a single dose. But it has the same G6PD risk and is more expensive. It’s also not approved for pregnant women or children under 16. For most people, primaquine remains the standard because it’s cheaper, widely available, and well-studied over decades.
Still, if you have mild G6PD deficiency, your doctor might prescribe a lower dose of primaquine over a longer period - sometimes up to 14 days - to reduce risk. This is called “low-dose primaquine” and is used in places like Thailand and Brazil with good success.
Real-world examples: What went wrong
In 2023, a traveler returning from Cambodia developed severe anemia after taking primaquine. He had no family history of G6PD deficiency and assumed he was fine. The test came back positive only after he was hospitalized. His case wasn’t unique. A study from the UK Health Security Agency found that 1 in 5 patients prescribed primaquine in 2022 had no prior G6PD testing - and 12% of them developed moderate to severe hemolysis.
Another case involved a woman in Leeds who took primaquine after a trip to India. She had mild nausea but ignored it. Two days later, her urine turned dark. She waited another day before seeing a doctor. By then, her hemoglobin had dropped dangerously low. She needed a blood transfusion. Her story highlights a dangerous myth: “If I feel okay, it’s fine.” Side effects can sneak up fast.
When to get help - and what to tell your doctor
Don’t wait for symptoms to get bad. If you’re on primaquine and notice:
- Unusual tiredness that doesn’t go away
- Dark urine
- Yellow eyes or skin
- Shortness of breath during normal activity
Call your doctor or go to urgent care. Tell them: “I’m taking primaquine and I’m worried about side effects.” That phrase alone will trigger the right checks - G6PD levels, liver enzymes, hemoglobin count.
Many doctors don’t ask about ancestry or drug history unless prompted. Be your own advocate. Bring a list of all medications, supplements, and recent travel. Don’t assume they know what you’ve been through.
Final thoughts: Primaquine is powerful - but not risk-free
Primaquine saves lives by stopping malaria from coming back. But it’s not a benign pill. It’s a tool that needs careful handling. The risks are real, predictable, and preventable - if you get tested, listen to your body, and speak up.
If your doctor skips the G6PD test, ask why. If you feel off after starting the drug, don’t brush it off. Your health isn’t worth gambling with.
Can I take primaquine if I have anemia?
No - if you already have anemia, primaquine can make it worse. It causes red blood cells to break down, which lowers hemoglobin further. If you have anemia from any cause - iron deficiency, chronic disease, or G6PD deficiency - your doctor should treat the root issue before considering primaquine. Always get a full blood count before starting.
Is primaquine safe during pregnancy?
No. Primaquine can harm the developing fetus, especially in the first trimester. It crosses the placenta and may cause severe anemia in the baby if the fetus has G6PD deficiency - which can’t be tested for until birth. Pregnant women with malaria are usually treated with chloroquine or other safer alternatives. Always tell your doctor if you’re pregnant or planning to be.
Can I drink alcohol while taking primaquine?
It’s best to avoid alcohol. While there’s no direct interaction, alcohol stresses your liver and can worsen nausea or dizziness from primaquine. It also increases the risk of dehydration, which makes side effects like kidney strain more likely. Stick to water and avoid heavy drinking during treatment.
How long do primaquine side effects last?
Common side effects like nausea or headache usually fade within a few days as your body adjusts. But if you develop signs of hemolysis - dark urine, jaundice, extreme fatigue - those symptoms can last weeks and may require hospital treatment. The drug stays in your system for about 3 days, but the damage to red blood cells can take longer to repair.
Are there natural alternatives to primaquine?
No. There are no proven natural or herbal alternatives that can kill dormant malaria parasites in the liver. Supplements like quinine from cinchona bark or artemisinin from sweet wormwood don’t work the same way and won’t prevent relapses. Relying on them instead of primaquine can lead to life-threatening malaria returning months later. Always follow medical advice - natural doesn’t mean safe or effective here.
Can I get tested for G6PD deficiency before traveling?
Yes - and you should. Many travel clinics offer G6PD testing before prescribing primaquine. The test is a simple blood draw that takes less than 10 minutes. Results are usually ready in 1-2 days. If you have ancestry from malaria-endemic regions or have had unexplained anemia in the past, get tested even if you’ve never taken primaquine. It’s a one-time check that could prevent a medical emergency.
If you’re planning travel to a malaria zone, talk to your doctor at least 4-6 weeks ahead. Don’t wait until you’re packing your bags. Primaquine isn’t something to rush into. It’s a medication that demands respect - and a little caution goes a long way.



Hannah Machiorlete, November 20, 2025
Primaquine is basically a medical gamble if you don’t get tested. My cousin took it after a trip to Thailand and ended up in the ER with dark urine and a hemoglobin level of 5. They didn’t even ask about his ancestry. Just handed him the script. Now he’s on iron supplements forever. Don’t be him.
Bette Rivas, November 21, 2025
It’s critical to emphasize that G6PD deficiency is not a rare condition globally-it affects approximately 400 million people, primarily in populations with African, Mediterranean, or Southeast Asian ancestry. The drug’s mechanism of action induces oxidative stress in red blood cells, which those lacking sufficient G6PD enzyme cannot neutralize, leading to intravascular hemolysis. This is not an allergic reaction-it’s a pharmacogenetic phenomenon. Standard pre-treatment screening with a quantitative G6PD assay, not just a rapid diagnostic test, is the gold standard. Many primary care providers still rely on outdated protocols or assume family history is sufficient, which is dangerously inadequate. The UK Health Security Agency’s 2022 data showing 20% of patients received primaquine without testing is a systemic failure, not an isolated error.
prasad gali, November 23, 2025
Let’s be clear-primaquine is not a ‘medication’ for the untested. It’s a chemical weapon against your own erythrocytes if you’re G6PD-deficient. The fact that clinicians still skip testing is criminal negligence. You don’t prescribe warfarin without checking INR. You don’t give penicillin without asking about allergies. Why is primaquine treated like candy? The WHO has clear guidelines. The CDC has bulletins. If your doctor hasn’t ordered a G6PD test, they’re either lazy or incompetent. Demand the test. Or don’t take it. There’s no middle ground.
Paige Basford, November 24, 2025
Okay but I just read that some people get really weird taste buds changes with primaquine-like everything tastes metallic or like pennies? My aunt said that happened to her and she thought she was dying, but it was just the drug. Also, I heard you should avoid citrus? Is that true? I’m planning a trip to Vietnam next month and I’m kinda nervous now lol. Maybe I should just get tested even if I feel fine? I mean, I’m half Filipino so… yikes.
Danielle Mazur, November 25, 2025
Primaquine is not just a drug-it’s part of a larger pharmaceutical agenda to profit off of preventable health crises. The G6PD test is cheap, but they don’t push it because it reduces prescriptions. The FDA, WHO, and CDC all have ties to Big Pharma. Look at the history: chloroquine was pulled because it was too safe and cheap. Now we have primaquine-expensive, risky, and dependent on testing that’s rarely done. Who benefits? The labs that charge for the test. The hospitals that treat the hemolytic crises. The pharmacies that sell the pills. It’s a perfect cycle. If you’re traveling, get tested. But also ask: why is this even necessary in the first place?
Margaret Wilson, November 27, 2025
Primaquine: the ‘I’m just gonna take this pill because the doctor said so’ trap. 😅 One minute you’re sipping coconut water in Bali, next minute you’re in a hospital with yellow eyes and a nurse asking if you’ve ever heard of G6PD. Spoiler: you hadn’t. And now you’ve got a scar on your body and a story you’ll tell at every family BBQ for the next decade. Don’t be the meme. Get tested. Like, yesterday. 🙏
william volcoff, November 27, 2025
Interesting that tafenoquine is presented as a ‘better’ alternative. It’s not. It’s just a longer-acting version of the same problem. Still causes hemolysis. Still contraindicated in pregnancy. Still requires G6PD testing. The real win would be developing a non-oxidative radical cure-but that’s not profitable enough for pharma. Also, the ‘low-dose primaquine’ protocol is actually brilliant. Used in Thailand for over a decade with near-zero hemolysis rates. Why isn’t this standard in the US? Because we’re allergic to nuanced dosing. We want one pill, one day, no thinking. But malaria isn’t that simple.
Freddy Lopez, November 28, 2025
Primaquine forces us to confront a fundamental truth: medicine is not neutral. It is a tool that reflects our values, our systems, and our failures. To prescribe it without testing is not ignorance-it is structural violence against those whose biology doesn’t fit the majority model. The fact that 400 million people carry G6PD deficiency, and yet screening remains optional in many places, reveals a deeper ethical crisis. We treat genetic risk as an afterthought, not a priority. Perhaps the real question isn’t ‘Is primaquine safe?’ but ‘Why do we accept systems that make safety conditional?’