Imagine trying to listen to someone whisper, but all you hear is muffled noise. Or sitting in a quiet room, and suddenly you can’t hear the low hum of a refrigerator-until you realize it’s not the fridge. It’s your own hearing slipping away. This is the reality for many people with otosclerosis, a quiet but progressive condition that hijacks sound by locking up a tiny bone in the middle ear.
What Exactly Is Otosclerosis?
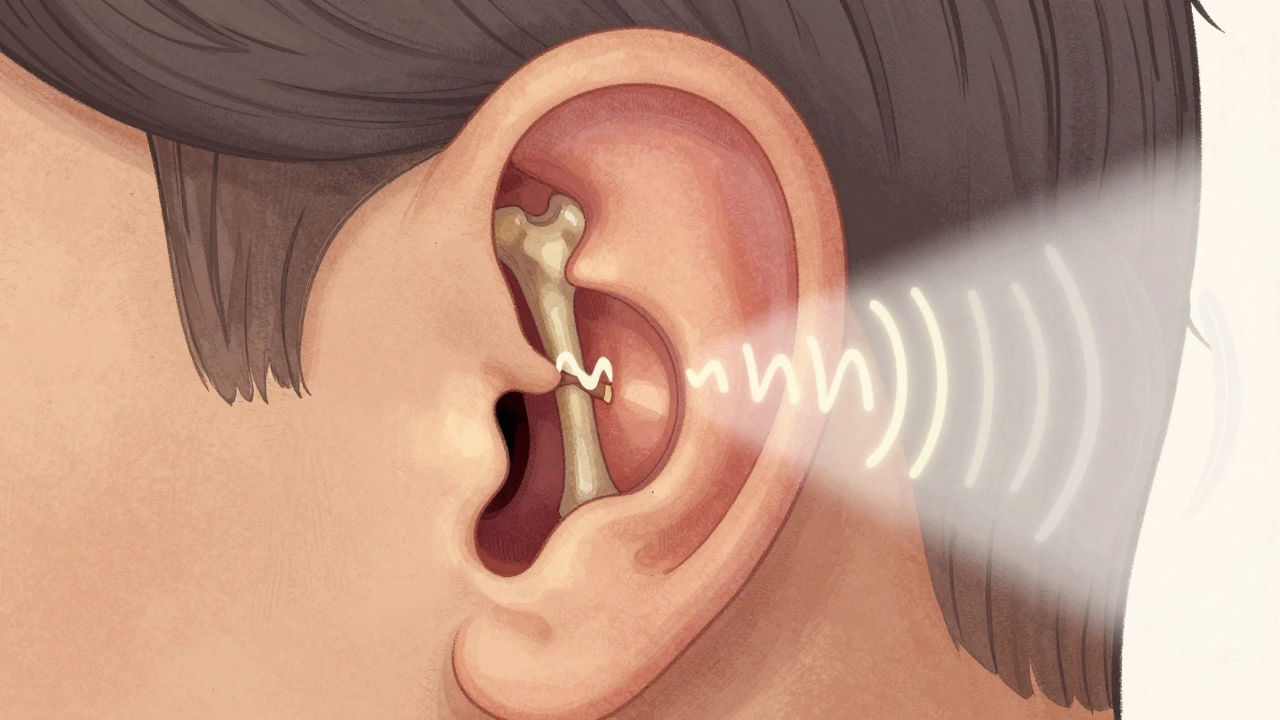
Otosclerosis is not a tumor. It’s not an infection. It’s abnormal bone growth-specifically, the body’s own bone cells going rogue inside the middle ear. The target? The stapes, the smallest bone in the human body, about the size of a grain of rice. This bone is supposed to vibrate like a drumstick tapping a tambourine, passing sound from the eardrum to the inner ear. But in otosclerosis, new bone forms around the stapes, fusing it to the oval window-the doorway to the inner ear. Once it’s stuck, it can’t move. Sound doesn’t get through. This isn’t sudden. It creeps in over years. People often notice it first when they struggle to hear low-pitched voices-like a man speaking or the bass in music. They might think their partner is mumbling, or that the TV volume is too low. But it’s not the sound. It’s the bone.Who Gets Otosclerosis?
It’s not random. About 1 in 200 people in the UK have it. In the U.S., that’s roughly 3 million people. It’s most common in adults between 30 and 50. And women are far more likely to be affected-about 70% of cases. Why? Hormones may play a role. Many women first notice symptoms during pregnancy, when hormonal shifts seem to speed up the bone remodeling process. Genetics matter too. If a parent or sibling has otosclerosis, your risk doubles. Researchers have found at least 15 genetic links, with the RELN gene on chromosome 7 being the strongest. It’s not a simple inherited trait, but if you have a family history, you’re definitely in a higher-risk group. Ethnicity also plays a part. Otosclerosis is most common in people of European descent, less common in Asians, and rarest in African populations. That pattern has held for decades, even as global mobility has increased.How It’s Diagnosed
Most people don’t go straight to an ear specialist. They start with their family doctor, who might suspect an ear infection or Eustachian tube dysfunction. In fact, about 22% of otosclerosis patients wait an average of 18 months before getting the right diagnosis. The key is a hearing test-pure-tone audiometry. This test shows a clear gap between air conduction (sound through the ear canal) and bone conduction (sound through the skull). In otosclerosis, this gap is usually between 20 and 40 decibels. Speech tests usually come back normal, which helps rule out nerve damage. That’s a big clue: if you can understand words clearly but can’t hear them loudly enough, it’s likely a mechanical blockage-not a nerve problem. Sometimes, a CT scan of the temporal bone reveals the telltale signs: small, dark spots where the abnormal bone is forming around the stapes. These foci are only 0.5 to 2.0 mm wide, but they’re enough to stop a bone from vibrating.How It’s Different From Other Hearing Losses
Not all hearing loss is the same. Otosclerosis stands out because of what it affects and how it progresses. - Noise-induced hearing loss hits high frequencies first-think bird songs, alarms, or the “s” sound in speech. Otosclerosis targets low frequencies, making voices sound dull or distant. - Presbycusis, or age-related hearing loss, usually starts after 65 and affects high pitches. Otosclerosis hits younger adults and hits low pitches. - Meniere’s disease comes with vertigo, ringing, and fluctuating hearing. Otosclerosis? Steady decline. No spinning. No sudden changes. This distinction matters because treatment depends on the cause. You wouldn’t use surgery for noise-induced loss. But for otosclerosis? Surgery is often the best fix.
What Happens If It’s Left Untreated?
Left alone, otosclerosis doesn’t just stay the same. It gets worse. On average, untreated cases lose 15 to 20 decibels of hearing over five years. That’s not just a little quieter. It’s the difference between hearing a conversation at arm’s length and needing someone to shout. In 10 to 15% of cases, the abnormal bone growth spreads to the inner ear-the cochlea. This turns a conductive hearing loss (mechanical) into a mixed or even sensorineural loss (nerve damage). Once the inner ear is involved, hearing aids become less effective, and surgery won’t help that part. Tinnitus is another common companion. Around 80% of people with otosclerosis report ringing or buzzing in the ears. For 35% of them, it’s bad enough to disrupt sleep. That’s not just about hearing-it’s about quality of life.Treatment Options: Hearing Aids vs. Surgery
There are two main paths: amplification or repair. Hearing aids are the first step for many. They don’t fix the bone-they just make sound louder. About 65% of patients start here. Modern digital aids can be programmed to boost low frequencies specifically, which helps a lot. But they don’t stop the disease. And some people hate the way their own voice sounds when amplified-the “occlusion effect,” where your voice booms inside your head. Surgery is the only way to fix the problem at its source. The gold standard is stapedotomy. Instead of removing the entire stapes (stapedectomy), surgeons drill a tiny hole in the footplate and insert a prosthetic piston-often made of titanium or platinum. This piston connects the incus (another middle ear bone) to the inner ear, bypassing the fused stapes. The eardrum stays intact. Recovery is quick: most people go home the same day. Success rates? Around 90-95%. In 87% of cases, patients achieve functional hearing-meaning they can hear normal conversation without aids. One 45-year-old teacher in Florida said after her surgery, “I can finally hear my students whispering in the back row.” But surgery isn’t risk-free. About 1% of patients experience sudden, permanent sensorineural hearing loss in the operated ear. That’s rare-but devastating. That’s why informed consent is critical. You need to know the odds before you sign.What’s New in Treatment?
The field isn’t standing still. In March 2024, the FDA approved a new prosthesis called StapesSound™. It’s coated with titanium-nitride, which reduces scar tissue and adhesions after surgery. Early trials show a 94% success rate at one year-up from 89% with older models. There’s also promising drug research. Sodium fluoride, long used for osteoporosis, is now being tested to slow bone growth in otosclerosis. A 2024 study found patients taking it had 37% less hearing decline over two years compared to those on placebo. It’s not a cure, but it might buy time-especially for people who aren’t ready for surgery. The biggest future shift? Genetic screening. Researchers are working on polygenic risk scores that could identify high-risk individuals before symptoms even appear. Within five years, we might be able to test young adults with a family history-and start monitoring or even intervening early.
Why Fewer Surgeons Are Doing It
Here’s the catch: stapedotomy is a highly specialized procedure. It requires precision under a microscope, deep knowledge of middle ear anatomy, and years of training. Mount Sinai requires surgeons to complete 50 supervised cases before they’re allowed to operate alone. But fewer young otolaryngologists are choosing to specialize in this. Many are focusing on cochlear implants or head and neck cancer. As a result, stapedectomy procedures in the U.S. have dropped 15% since 2018. That means access is becoming harder in some areas. If you’re diagnosed, you may need to travel to find a surgeon with the right experience.Living With Otosclerosis
If you’ve been diagnosed, you’re not alone. The Hearing Loss Association of America has over 1,200 members in its otosclerosis support group. Many report the same struggles: avoiding phone calls, turning up the TV too loud, feeling isolated in group conversations. But the outlook is hopeful. With early diagnosis, most people can keep their hearing functional for life. Whether through hearing aids, surgery, or a combination, the vast majority regain the ability to connect with the world around them. The key is not to wait. If you’ve had unexplained hearing loss for more than six months-if low voices sound muffled, if you’re constantly asking people to repeat themselves-get your hearing tested. Don’t assume it’s just aging. It might be something fixable.When to See a Specialist
See an otolaryngologist (ear, nose, and throat doctor) if:- Your hearing loss is worse in one ear
- You notice difficulty hearing low-pitched sounds
- You have a family history of hearing loss
- You’ve had tinnitus for more than a few weeks
- Audiometry shows an air-bone gap
Is otosclerosis the same as earwax blockage?
No. Earwax blockage is a simple, temporary issue caused by buildup in the ear canal. It’s easily cleared by a doctor and doesn’t involve bone growth. Otosclerosis is a structural problem inside the middle ear, involving abnormal bone remodeling around the stapes. It’s not removable with irrigation or drops.
Can otosclerosis cause complete deafness?
Rarely. Otosclerosis usually causes conductive hearing loss, which means sound can’t reach the inner ear-but the inner ear itself is still working. Even in advanced cases, total deafness is uncommon. With treatment-either hearing aids or surgery-90% of patients regain functional hearing. Only when the disease spreads to the cochlea does the risk of permanent sensorineural loss increase.
Is surgery always necessary for otosclerosis?
No. Many people manage well with hearing aids, especially if the hearing loss is mild or they’re not ready for surgery. Surgery is typically recommended when hearing loss reaches 30-40 dB and begins to interfere with daily life. Some patients choose to monitor the condition for years before deciding. The choice depends on lifestyle, severity, and personal comfort with risk.
Does pregnancy make otosclerosis worse?
Yes. Hormonal changes during pregnancy can accelerate bone remodeling, which may speed up the progression of otosclerosis. Many women first notice hearing loss during or after pregnancy. If you have otosclerosis and are planning a pregnancy, it’s wise to get a baseline hearing test and discuss management options with your doctor ahead of time.
Can otosclerosis come back after surgery?
The bone growth itself doesn’t typically return after a successful stapedotomy. However, complications like scar tissue or prosthesis displacement can cause hearing to decline again. Revision surgery is possible but less successful-around 75% effective compared to 95% for the first procedure. That’s why choosing an experienced surgeon matters so much.
Are there any home remedies or supplements that help?
No. There’s no evidence that vitamins, herbs, or home remedies can stop or reverse otosclerosis. Some people try sodium fluoride supplements, but this is only done under medical supervision as part of a clinical protocol-not as an over-the-counter solution. The only proven treatments are hearing aids and surgery.



James Kerr, December 3, 2025
Man, I had no idea this was even a thing. My mom’s been struggling to hear my dad for years, and we thought it was just old age. Guess we should’ve pushed for an audiogram sooner. Thanks for laying this out so clearly. 🙌
shalini vaishnav, December 4, 2025
Typical Western medical reductionism. In India, we’ve known for centuries that hearing loss stems from imbalanced doshas-especially Vata. No need for titanium pistons when Ayurveda can restore equilibrium. This post reads like corporate propaganda disguised as science.
bobby chandra, December 6, 2025
Let me tell you-this isn’t just a medical condition, it’s a silent revolution in how we think about sound. That tiny stapes bone? It’s the unsung hero of human perception. And when it gets locked up? It’s like your ears are trapped in a soundproof vault. But here’s the kicker: modern stapedotomy isn’t surgery-it’s sonic liberation. You don’t just hear better. You feel alive again. That Florida teacher? She didn’t just get her hearing back-she got her classroom, her joy, her humanity. And that’s worth every risk.
Archie singh, December 6, 2025
Hearing aids are a bandaid. Surgery is the only real solution. If you're not willing to risk 1% permanent loss to regain 90% of your life you're not living you're just existing. Stop being scared and get it done. Period.
Gene Linetsky, December 7, 2025
Did you know the FDA approved that new prosthesis right after a secret meeting with Big Hearing Aid? The whole thing’s a money grab. Sodium fluoride? That’s the same stuff they used to put in water to suppress thyroid function. And don’t get me started on the ‘genetic screening’ push-they want to label kids as ‘high risk’ before they even speak. This isn’t medicine. It’s control.
Ignacio Pacheco, December 8, 2025
So let me get this straight-you’re telling me the same bone that lets me hear my kid’s laugh is also the reason I can’t tell if my dog’s barking or the neighbor’s garbage truck? And the cure is drilling a hole in it and sticking a metal rod in? That’s wild. I mean… it works? Like, really? I feel like I just watched a sci-fi movie.
Jim Schultz, December 9, 2025
Wow. Just… wow. You wrote a 2,000-word essay on otosclerosis, and yet you completely ignored the elephant in the room: the fact that ENT specialists are abandoning this procedure because it’s too niche, too low-revenue, and too damn hard. This isn’t about science-it’s about economics. Hospitals don’t care if you can hear your wife whisper-they care if you’ll pay for a cochlear implant next year. The real tragedy? The system’s designed to let you suffer until you’re desperate enough to pay for the fix.
Kidar Saleh, December 9, 2025
I’ve seen this in my clinic in London-women in their late 30s, first noticed it after their second child. Quiet. Embarrassed. Thinking it’s just fatigue. The stigma around hearing loss is still alive, even here. But what struck me most? The moment they hear their own child’s voice clearly again after surgery. It’s not just medical. It’s emotional. It’s the sound of connection restored. If you’re reading this and you’re unsure-don’t wait. Your family needs you to hear them.
Joykrishna Banerjee, December 10, 2025
Interesting. But let’s be real-this entire paradigm is built on Western biomedical hegemony. In Bengal, we treat this with Kshara Sutra therapy and Nasya. The stapes isn’t ‘fused’-it’s an expression of Ama accumulation. Your ‘prosthetic piston’ is just a crude mechanical workaround. The real solution? Detoxification. Diet. Pranayama. You’re treating the symptom, not the root. And frankly, your reliance on titanium is… gauche.