What Biologic DMARDs Really Do for Rheumatoid Arthritis
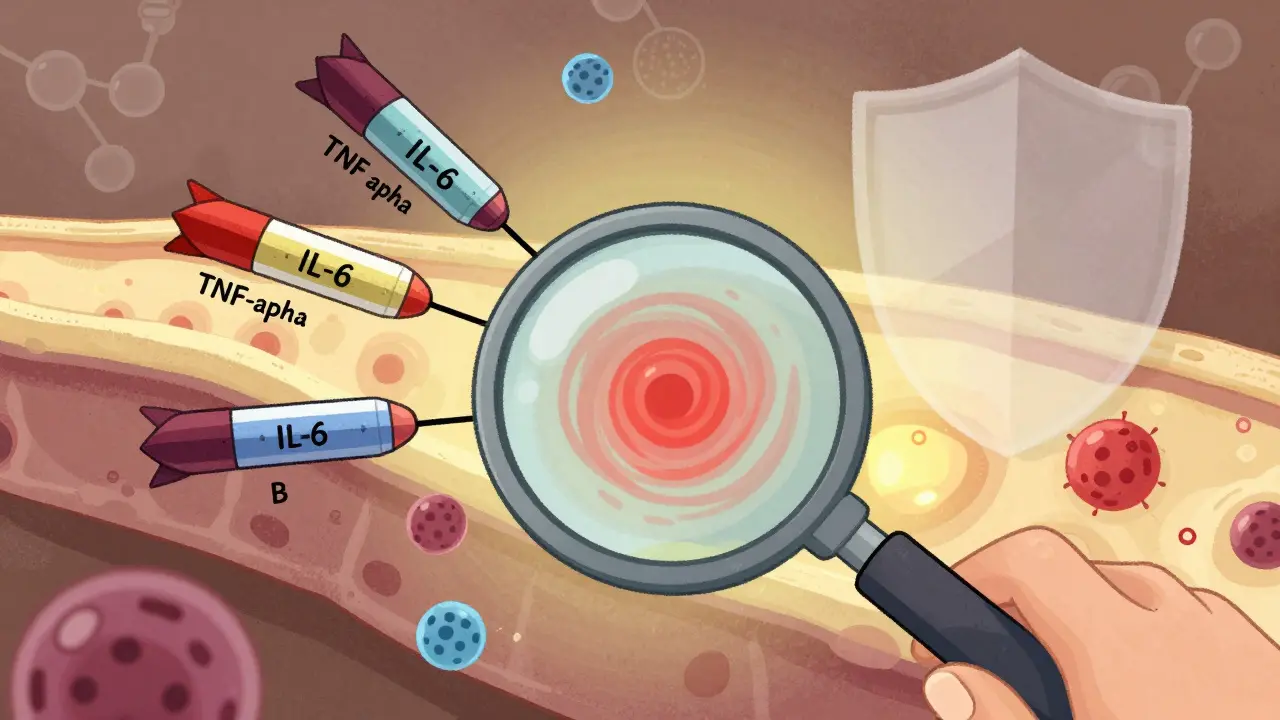
For decades, rheumatoid arthritis (RA) was seen as a slow, inevitable march toward joint destruction. But since the late 1990s, when the first biologic DMARD hit the market, that story has changed. Biologic DMARDs don’t just ease pain-they stop the immune system from attacking your own joints. These aren’t your grandpa’s arthritis pills. They’re targeted drugs, designed like precision missiles to block specific parts of the immune response that cause inflammation. Unlike older drugs like methotrexate, which broadly suppress the immune system, biologics pick their targets: TNF-alpha, IL-6, T-cells, or B-cells. And for many people, that’s the difference between living with pain and living without it.
Why Methotrexate Still Comes First
You might hear about biologics and think, ‘Why not start with the powerful stuff?’ But here’s the reality: methotrexate is still the foundation. It’s cheap, well-studied, and works for a lot of people. The American College of Rheumatology says most RA patients should start with methotrexate before jumping to biologics. Why? Because about 60-70% of people get good control with it alone. Only if your symptoms don’t improve after 3-6 months-despite taking methotrexate at the right dose-do doctors consider adding a biologic. It’s not about being ‘stronger’; it’s about being smart. Start with what works, then escalate only if needed.
The Big Five: Types of Biologic DMARDs
Not all biologics are the same. They fall into clear groups based on what they block:
- TNF inhibitors: These were the first. Drugs like etanercept (Enbrel), adalimumab (Humira), and infliximab (Remicade) block tumor necrosis factor, a major driver of inflammation. Most people get symptom relief within weeks.
- IL-6 blockers: Tocilizumab (Actemra) shuts down interleukin-6, another key inflammation signal. It’s especially helpful for people with high CRP levels or severe fatigue.
- T-cell modulators: Abatacept (Orencia) stops T-cells from getting activated. It’s slower to work but has a good safety profile.
- B-cell depleters: Rituximab (Rituxan) wipes out B-cells. It’s often used when TNF inhibitors fail, but only if your synovial tissue shows high B-cell activity.
- JAK inhibitors: Though technically synthetic, drugs like tofacitinib (Xeljanz) and upadacitinib (Rinvoq) work like biologics-targeting signals inside cells. They’re taken as pills, not injections.
Here’s the thing: what works for one person might not work for another. It’s not random-it’s biology. If your joint tissue has lots of B-cells, rituximab might be your best shot. If your inflammation is driven by IL-6, tocilizumab could be the key. That’s why some rheumatologists now test synovial fluid or blood markers before choosing a drug.
Remission Isn’t a Miracle-It’s a Target
Remission doesn’t mean you’re cured. It means your disease is quiet. No swelling. No pain. No joint damage creeping forward. And yes, it’s possible. Studies show 20-50% of people on biologics reach remission, compared to just 5-15% on methotrexate alone. But remission doesn’t happen by accident. It requires a clear goal: treat-to-target. That means your rheumatologist measures your disease activity every few months using tools like DAS28. If you’re not getting closer to remission in 3-6 months, they’ll switch or adjust your treatment. No waiting. No hoping. Just action.
Real People, Real Results-and Real Problems
On patient forums, stories pour in. One woman in Leeds started adalimumab after 12 years of pain. Within 8 weeks, she could hold her grandchild without wincing. Another man in Manchester switched to a biosimilar of etanercept and cut his monthly cost from £1,200 to £800. These aren’t outliers-they’re common outcomes.
But there’s a flip side. About 32% of people report side effects. Injection site redness? Common. A bad cold that won’t go away? That’s a red flag. Biologics increase your risk of serious infections like tuberculosis or pneumonia. That’s why you get screened before starting. And then there’s cost. In the U.S., a year of Humira can run $70,000. In the UK, the NHS covers it, but getting approval can take weeks. Biosimilars have helped-now 35% of TNF prescriptions in the U.S. are biosimilars, saving patients and systems millions.
And then there’s the long game. About 40% of people who start a biologic lose its effect after 1-2 years. That’s called secondary non-response. It’s not failure-it’s biology adapting. When that happens, switching to a biologic with a different mechanism (like going from a TNF inhibitor to a JAK inhibitor) often works. But each new drug tends to be less effective than the last. That’s why getting the first one right matters more than you think.
How to Actually Use These Drugs
Most biologics are injected under the skin. Sounds scary? Most people learn in 1-2 sessions with a nurse. You’ll get training on how to store them (some need refrigeration), how to rotate injection sites, and how to handle the auto-injector. About 75% of patients master it without help after two tries.
Infusions like infliximab mean going to a clinic every 4-8 weeks. That’s time out of your day, but some people prefer it-no needles at home. Either way, you’ll need regular blood tests to check liver function, blood counts, and signs of infection. You’ll also need to know the warning signs: fever, chills, new cough, unexplained bruising. Call your doctor immediately if you see any of those.

What’s Next? The Future of RA Treatment
The next five years will change how we treat RA. Biosimilars are exploding-by 2027, they could make up 60% of biologic use. That means more people will get access. Longer-acting drugs are coming too. A twice-yearly version of tocilizumab is in late-stage trials. Imagine one injection every six months instead of weekly.
And the biggest shift? Personalization. Scientists are starting to match drugs to patients based on their immune profile. If your blood shows high IL-6, you get tocilizumab. If your joint tissue is full of B-cells, you get rituximab. This isn’t science fiction-it’s happening in research clinics now. The goal isn’t just to treat RA. It’s to predict who will respond to what, before you even start.
When Biologics Aren’t the Answer
Not everyone needs them. Mild RA? Maybe methotrexate and physical therapy are enough. If you’re over 70 and have other health issues, your doctor might avoid biologics because of infection risks. If you’re pregnant or planning to be, some biologics are safer than others-but none are risk-free. And if cost is a barrier and you’re outside the U.S. or Europe, access is still limited. In many low-income countries, fewer than 10% of RA patients get biologics at all.
That’s why the goal isn’t just to push biologics. It’s to make sure the right person gets the right drug at the right time. Not more drugs. Better choices.
Can biologic DMARDs really put rheumatoid arthritis into remission?
Yes, they can. Studies show that 20-50% of people with RA achieve remission when using biologic DMARDs, especially when combined with methotrexate. Remission means no visible joint swelling, no pain, and no ongoing damage seen on scans. It’s not a cure, but it’s the closest thing to one we have today. The key is sticking with treatment and working with your rheumatologist to adjust if needed.
Why do some people stop responding to biologics over time?
This is called secondary non-response. It happens in about 40% of patients after 12-24 months. The immune system can adapt-building antibodies against the drug or changing the inflammation pathways it uses. It doesn’t mean the drug failed; it means your body changed. Switching to a biologic with a different target (like going from a TNF blocker to a JAK inhibitor) often restores control. That’s why doctors don’t keep trying the same drug over and over.
Are biosimilars as good as the original biologics?
Yes, they are. Biosimilars are not generics-they’re highly similar versions made after the original patent expires. They undergo strict testing to prove they work the same way, with the same safety profile. In the U.S., 35% of TNF inhibitor prescriptions are now biosimilars. Patients report similar effectiveness and side effects. The big difference? Cost. Biosimilars can save patients 15-30% on out-of-pocket expenses.
How long does it take to feel better on a biologic?
It varies. TNF inhibitors like adalimumab or etanercept often bring relief in 2-4 weeks. Others, like abatacept or rituximab, can take 3-6 months to show full effect. Don’t give up if you don’t feel better right away. Your doctor will track your progress with blood tests and joint exams. If you’re not improving after 3 months, they’ll likely adjust your treatment plan.
Do I need to stay on biologics forever?
Most people do, but not always. If you achieve deep, lasting remission (usually after 6-12 months), your doctor might try slowly lowering the dose. Some people can stop entirely and stay in remission-but that’s rare, and only happens under close monitoring. Stopping without guidance can cause a flare. Never stop a biologic on your own. Always work with your rheumatologist.
What are the biggest risks of biologic DMARDs?
The biggest risk is serious infection-like pneumonia, tuberculosis, or sepsis. That’s why you’re tested for TB before starting. Other risks include reactivation of hepatitis, rare nervous system disorders, and possibly higher rates of certain cancers (though evidence is mixed). Injection site reactions are common but mild. Most side effects are manageable with monitoring. The benefit of preventing joint damage usually outweighs the risks-for the right patient.
What to Do Next
If you’re on methotrexate and still in pain, talk to your rheumatologist about your disease activity score. Ask if you’re a candidate for a biologic. If you’re already on one and not improving, ask: ‘Is this the right drug for my type of RA?’ Bring your symptom diary. Ask about biosimilars if cost is an issue. And if you’re unsure where to start, look into patient support tools like ArthritisPower or MyRApath-they help track symptoms and meds, and connect you with resources.
RA isn’t a life sentence anymore. With the right treatment, remission is possible. But it takes the right drug, the right timing, and the right partnership with your doctor. Don’t settle for just managing pain. Aim for remission. It’s not a dream-it’s a medical reality now.



Eli Kiseop, February 1, 2026
I swear biologics changed my life but also made me paranoid every time I get a cold
like bro is this just a sinus thing or is my immune system finally giving up?
Ellie Norris, February 3, 2026
ohhh i switched to the biosimilar of humira last year and my wallet cried happy tears 😭 like 1200 to 80 a month? yes please. also my knees stopped sounding like popcorn machine
Marc Durocher, February 4, 2026
so let me get this straight
we got these $70k/year miracle drugs that work great
but we start with methotrexate because it's cheap?
and then we wait 6 months to see if it works?
and if it doesn't we try the expensive one?
and if THAT fails we switch to another expensive one?
and if THAT fails we're basically just waiting to die?
...yep. american healthcare in a nutshell.
larry keenan, February 4, 2026
The clinical data supporting treat-to-target protocols with DAS28 monitoring demonstrates statistically significant improvement in radiographic progression inhibition when biologic DMARDs are initiated following inadequate response to conventional synthetic DMARDs. The risk-benefit profile remains favorable for appropriately screened patients.
Akhona Myeki, February 5, 2026
In South Africa we don't even have access to methotrexate in rural clinics. You talk about biologics like they're candy. We're lucky if we get a paracetamol prescription without a 3-month waiting list. This is not medicine. This is a luxury for the wealthy. The world is broken.
Chinmoy Kumar, February 6, 2026
i had abatacept for 2 years and it was so slowww but when it hit? man i could hold my dog again without crying
took 5 months but worth it
also my mom said i looked younger like i stopped aging for a bit lol
jay patel, February 8, 2026
so you're telling me that after 18 months of the same biologic i'm supposed to just switch to another one because my body got bored?
like what if i just... don't?
what if i just learn to live with the pain?
because honestly the thought of another injection, another blood test, another doctor who talks like a textbook... i'm just tired.
and yeah i know i'm not supposed to say that but i'm saying it anyway.
phara don, February 9, 2026
JAK inhibitors are wild. Pill instead of shot? Yes please 🙌
also why does everyone act like TB screening is a joke? I got a chest x-ray and a blood test and then a 3-week wait for results. I felt like a spy.
Bob Hynes, February 9, 2026
i moved from the US to Canada and the difference in access is like night and day
here they just give you the drug. no paperwork. no begging. no $70k bills
and yet... i still feel guilty taking it
like someone else in India probably needs it more
and i'm just sitting here with my auto-injector and my free prescription
weird how medicine can be both a miracle and a moral crisis at the same time
Vatsal Srivastava, February 10, 2026
Biologics? Please. All this is just placebo with a fancy name. The real cure is diet. And fasting. And yoga. And cold showers. But no, let's just inject money into pharma instead of actually thinking. You're all just sheep.