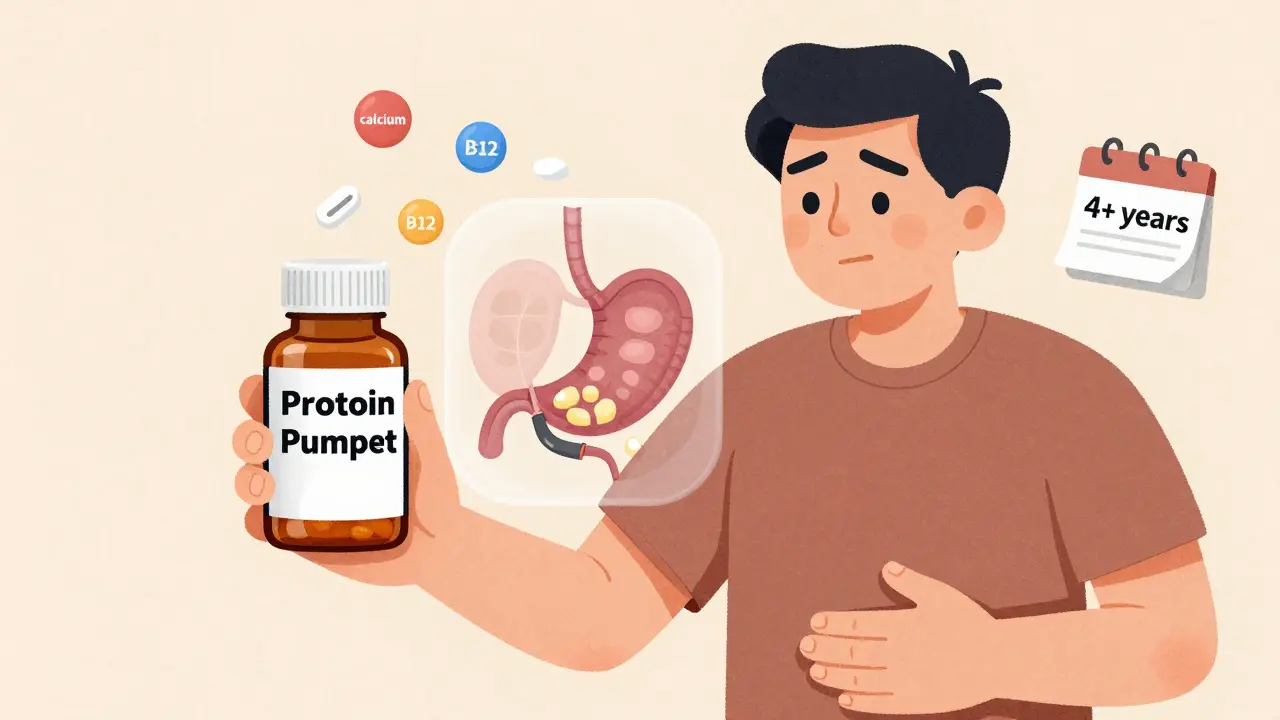
Millions of people take proton pump inhibitors (PPIs) every day-omeprazole, esomeprazole, pantoprazole-to manage heartburn, acid reflux, or stomach ulcers. They work fast, they work well, and for many, they feel like a miracle. But what happens when you take them for months? Years? The truth is, PPIs aren’t harmless. And if you’ve been on them longer than a few weeks, you might be at risk for problems you never knew about.
How PPIs Work (And Why They’re So Popular)
PPIs block the proton pumps in your stomach lining-the tiny engines that produce acid. By shutting them down, they cut acid production by more than 90%. That’s why they’re the gold standard for healing erosive esophagitis and treating severe GERD. Compared to H2 blockers like famotidine (Pepcid), PPIs heal ulcers and inflammation much faster and more completely.
But here’s the catch: they’re not meant to be taken forever. The FDA says over-the-counter PPIs should only be used for 14 days, no more than once every three months. Yet, a 2023 study in US Pharmacist found that 7 million Americans use OTC PPIs longer than that-often without ever talking to a doctor. Prescription use is even more widespread: 15 million people in the U.S. take PPIs daily, many for years.
The Real Long-Term Risks
The FDA has issued seven safety warnings about PPIs since 2010. Some risks are rare. Others are more common than you think.
- Fractures: Long-term PPI use (especially over 4 years) increases hip fracture risk by up to 55%. Why? Acid helps your body absorb calcium. Less acid means less calcium gets into your bones. The risk goes up the longer you take them-but it reverses if you stop. Women who quit PPIs more than two years ago had fracture rates similar to those who never took them.
- Magnesium deficiency: This one’s serious but rare. Only about 0.5-1% of long-term users develop it. But when it happens, it can cause muscle cramps, irregular heartbeat, seizures, or even cardiac arrest. The FDA now recommends checking magnesium levels if you’ve been on PPIs for over a year.
- Vitamin B12 deficiency: Up to 15% of people on PPIs for more than two years become deficient. B12 is critical for nerve function and red blood cell production. Symptoms like fatigue, numbness, memory issues, or depression can be mistaken for aging-or stress-when they’re actually from low B12.
- C. difficile infection: PPIs raise your risk of this dangerous gut infection by 1.7 to 2 times. It’s especially risky in hospitals or nursing homes. The infection causes severe diarrhea, fever, and can be life-threatening.
- Acute interstitial nephritis: A rare kidney inflammation that can lead to permanent damage. The FDA flagged this in 2016. While most cases reverse after stopping PPIs, some patients develop chronic kidney disease.
What about dementia, heart disease, or stomach cancer? Studies have linked PPIs to these conditions-but the evidence is shaky. Many of those studies didn’t control for other factors. People on long-term PPIs often have other health problems: obesity, diabetes, smoking, poor diet. It’s hard to say if the PPI caused the problem-or if it’s just a side effect of the lifestyle behind it. Experts like Dr. William Ravich at Yale Medicine say: "Many of the studies linking PPIs to dementia or heart disease weren’t focused on PPIs at all. They were studying other things, and PPI use was just a side note."
Rebound Acid: The Hidden Trap
If you’ve tried to stop PPIs and ended up with worse heartburn than before, you’re not crazy. This is called rebound acid hypersecretion. It happens in 40-80% of people who’ve taken PPIs for more than a few months.
Why? Your stomach gets used to low acid. When you suddenly stop, the proton pumps go into overdrive, pumping out way more acid than normal. It can last for weeks. Many people think their reflux is back-and they go right back on the PPI. But it’s not the disease returning. It’s your body adjusting.
That’s why quitting cold turkey doesn’t work. You need a plan.

When and How to Stop
Not everyone needs to stop. If you have Barrett’s esophagus, a history of bleeding ulcers, or severe esophagitis-PPIs may be life-saving. But if you’re taking them for occasional heartburn, bloating, or "indigestion" without a confirmed diagnosis? You should reconsider.
The American College of Gastroenterology recommends trying to stop every 6-12 months. Here’s how:
- Reduce your dose. If you’re on 40mg, drop to 20mg. If you’re on 20mg, go to 10mg. Do this over 1-2 weeks.
- Switch to on-demand use. Instead of taking it daily, take it only when symptoms flare up. Use it for 3-5 days at a time, then stop.
- Try H2 blockers. Famotidine (Pepcid) or ranitidine (if available) can help manage breakthrough symptoms without the same long-term risks.
- Use antacids for quick relief. Tums, Rolaids, or Maalox work fast. They don’t fix the root cause, but they’re safe for occasional use.
- Give it time. Rebound symptoms usually fade after 2-8 weeks. Keep a journal. Track what you eat, when you take meds, and how you feel.
And never stop without talking to your doctor. If you’re on high-dose PPIs or have other health issues, your doctor may need to monitor you.
What Else Can You Do?
Medication isn’t the only answer. Lifestyle changes often work better-and with zero side effects.
- Don’t lie down after eating. Wait at least 3 hours. Gravity helps keep acid where it belongs.
- Watch your triggers. Coffee, chocolate, spicy food, alcohol, and large meals are common offenders. Keep a food diary for a week.
- Elevate your head while sleeping. Use a wedge pillow or raise the head of your bed by 6 inches.
- Loosen your belt. Tight clothes increase pressure on your stomach, pushing acid upward.
- Lose weight if needed. Even 5-10 pounds can make a big difference.
- Quit smoking. Smoking weakens the lower esophageal sphincter-the valve that keeps acid in.
What About Over-the-Counter PPIs?
They’re sold like candy. But they’re not safe for daily, long-term use. The FDA’s 14-day limit exists for a reason. If you need OTC PPIs more than once every three months, you need a doctor. Not a pharmacy shelf.
And don’t assume "natural" remedies work. Apple cider vinegar? Baking soda? These can make acid reflux worse. There’s no solid evidence they help. Stick with proven strategies: diet, weight, posture, and medical advice.
The Bottom Line
PPIs are powerful tools. But they’re not meant to be lifelong companions. If you’ve been on them for more than 8 weeks without a clear diagnosis-ask your doctor if you can try to stop. If you’ve been on them for years, it’s not too late. Many people successfully quit and never look back.
The goal isn’t to scare you off PPIs. It’s to make sure you’re not taking them longer than you need to. Because the safest dose of any medicine is the one you don’t take.
Can I stop taking PPIs cold turkey?
No. Stopping abruptly can cause severe rebound acid reflux, which may last for weeks. Instead, reduce your dose gradually over 1-2 weeks, then switch to on-demand use before stopping completely. Always consult your doctor first.
How long is too long to be on PPIs?
For most conditions like GERD or ulcers, 4-8 weeks is enough. If you still need them after that, your doctor should reassess whether you truly need daily therapy. Long-term use (over 1 year) increases risks like fractures, low magnesium, and B12 deficiency. Regular "drug holidays" every 6-12 months are recommended.
Are there safer alternatives to PPIs?
For occasional symptoms, H2 blockers like famotidine (Pepcid) are safer for long-term use. Antacids (Tums, Rolaids) work instantly and have no long-term risks. Lifestyle changes-weight loss, avoiding trigger foods, not lying down after meals-are often more effective than medication for mild reflux.
Do PPIs cause kidney damage?
PPIs can cause acute interstitial nephritis, a rare but serious kidney inflammation. This usually reverses after stopping the drug. There’s no strong evidence they cause chronic kidney disease, but long-term use should be monitored, especially in older adults or those with existing kidney issues.
Can PPIs lead to vitamin deficiencies?
Yes. Long-term use (over 2 years) can reduce absorption of vitamin B12 and magnesium. About 10-15% of long-term users develop B12 deficiency, which can cause nerve damage, fatigue, and memory problems. Magnesium deficiency is rarer but can be dangerous. Blood tests can detect these, and supplements can help if needed.
Why do doctors prescribe PPIs so often if they have risks?
PPIs are extremely effective for serious conditions like bleeding ulcers or severe esophagitis. They’re also easy to prescribe-patients feel better quickly. But overuse is common. Studies show up to 70% of prescriptions lack clear medical justification. Many are given for mild symptoms that could be managed with diet, lifestyle changes, or short-term use.



Carrie Schluckbier, February 16, 2026
Let me guess-Big Pharma paid off the FDA to make PPIs look harmless while they rake in billions. I’ve seen the leaked memos. They knew about the kidney damage and B12 crashes years ago. They just didn’t want you to know you could fix heartburn with a $3 wedge pillow and not taking pizza before bed. The real scandal? Doctors don’t even check your magnesium. They just keep writing scripts. Wake up, sheeple.
Liam Earney, February 18, 2026
Oh, I see… so now we’re supposed to believe that the human body, this miraculous, self-regulating, ancient machine-designed over millennia by evolution-is somehow incapable of handling its own acid production unless we intervene with synthetic proton pump inhibitors? I mean, really… have you ever considered that perhaps the real issue isn’t the acid… but the fact that we’ve turned our digestive tracts into a landfill of processed foods, caffeine, and emotional stress? And now, we’re medicating the symptom, not the soul? I’m not saying we should go full herbalist… but… perhaps… we should… ask… deeper questions?
guy greenfeld, February 18, 2026
They say ‘don’t take PPIs long-term’-but who’s really in charge here? The doctor? Or the algorithm that auto-suggests ‘PPI for heartburn’ when you type ‘stomach pain’ into Epic? I’ve been on omeprazole for 7 years. My doctor never asked why. Just refilled. Same as my statin. Same as my antidepressant. We’re not patients. We’re data points in a profit matrix. And now they want us to ‘wean off’? Like we’re addicts? Maybe we are. But who made us that way?
Sam Pearlman, February 20, 2026
I stopped my PPI cold turkey last year-no plan, no doctor, just said ‘screw it.’ First week? Brutal. Felt like lava in my throat. But by week 4? Gone. Better than ever. Now I eat tacos at midnight and sleep like a baby. Who knew? The body’s got its own back. You just gotta stop micromanaging it.
John Haberstroh, February 20, 2026
Rebound acid is wild, honestly. It’s like your stomach throws a tantrum because it’s been on vacation for years. I went from 40mg daily to 10mg, then to Pepcid on-demand. Took 3 months, but now I only need it when I eat too much cheese or cry over a Netflix show. The real win? I stopped feeling like a drug-dependent zombie. Also, I started drinking chamomile tea. It’s not magic, but it’s peaceful.
Logan Hawker, February 21, 2026
One must consider the epistemological framework of pharmaceutical interventionism. The PPI paradigm is not merely a pharmacological solution but a symptom of the neoliberal medical-industrial complex’s colonization of somatic autonomy. By pathologizing transient dyspepsia, we’ve commodified gastric distress, transforming visceral discomfort into a revenue stream for multinational conglomerates. The FDA’s 14-day limit is a performative gesture-a regulatory fig leaf. The true cure? A return to ancestral dietary patterns and somatic mindfulness.
James Lloyd, February 23, 2026
For anyone considering stopping PPIs: start by tracking your symptoms for 2 weeks without meds. Note meals, timing, posture. Then reduce dose by 50% for 10 days. Switch to H2 blocker every other day. Use antacids sparingly. Keep a log. If symptoms flare, pause. Don’t panic. Most people stabilize in 4-6 weeks. And yes-get your B12 and magnesium checked. Simple blood tests. Worth it.
Steph Carr, February 24, 2026
So let me get this straight-we’ve got a $12 billion industry built on convincing people that their stomach is broken… and the cure is to take a pill that makes their bones brittle, their nerves numb, and their gut vulnerable to infection? And we call this healthcare? I mean, if this was a car, we’d recall it. But nope. We call it ‘standard of care.’ Thanks, capitalism.
Tony Shuman, February 25, 2026
My uncle in Ohio took PPIs for 12 years. Broke his hip. Lost his B12. Got C. diff. Then he tried that ‘apple cider vinegar’ nonsense and ended up in the ER. America’s gone soft. We want magic pills for everything. Back in my day, we ate spicy food, drank coffee after dinner, and swallowed the burn. No pills. Just grit. And we didn’t die.
Haley DeWitt, February 26, 2026
OMG I JUST STOPPED MY PPI!! 😱 First 2 weeks were rough but now I’m like… I don’t even remember what heartburn felt like?? 🙌 I started walking after dinner and sleeping on my left side. Also, I stopped drinking soda. WHO KNEW?? 🥹✨
Adam Short, February 26, 2026
British NHS does this right. They screen you before prescribing. We don’t just hand out PPIs like candy. We ask: ‘Have you tried raising your bed? Are you eating late? Do you smoke?’ If you’re still on it after 8 weeks, you get referred. No magic. Just logic. Shame the US is still stuck in ‘pill for everything’ mode.
Prateek Nalwaya, February 27, 2026
As someone from India where turmeric, ginger tea, and chewing fennel seeds is the go-to for digestion, I find it funny how we’ve outsourced our gut health to a pill. My grandma never heard of PPIs. She had heartburn? A spoon of ghee + warm water. And she lived to 98. Maybe we lost something when we stopped listening to the body and started listening to ads.
Geoff Forbes, February 27, 2026
Ugh I hate when people say ‘just stop taking it’ like it’s easy. I have a hiatal hernia. I can’t just ‘eat better.’ I need the PPI. But my doctor won’t let me refill. Says I’m ‘overusing.’ Bro, I can’t sleep. I’m not a zombie. I’m a human with a broken valve. Chill.
Jonathan Ruth, March 1, 2026
Y’all act like PPIs are poison. They’re not. They’re tools. If you have Barrett’s or a bleeding ulcer, they save your life. Stop acting like every person on PPIs is a dumbass who eats nachos in bed. Some of us have real conditions. Not everyone can just ‘elevate their head’ and call it a day.
Philip Blankenship, March 1, 2026
I was on 40mg of pantoprazole for 5 years. Never thought twice. Then I started reading about the bone fractures and got scared. I cut down slowly over 6 months-switched to Pepcid at night, started sleeping upright. Took 3 months to feel normal again. My acid reflux? Gone. My energy? Better. My sleep? Deeper. I didn’t need the pill. I just needed to stop pretending my body was broken.