Herpes simplex virus isn’t just a cold sore you get once in a while. For millions, it’s a lifelong condition that shapes how they touch, kiss, and even think about intimacy. Two types - HSV-1 and HSV-2 - are responsible for most cases, and they don’t behave the same way. Understanding the difference isn’t just medical trivia; it affects how you treat it, how you protect others, and how you live with it.
What Are HSV-1 and HSV-2?
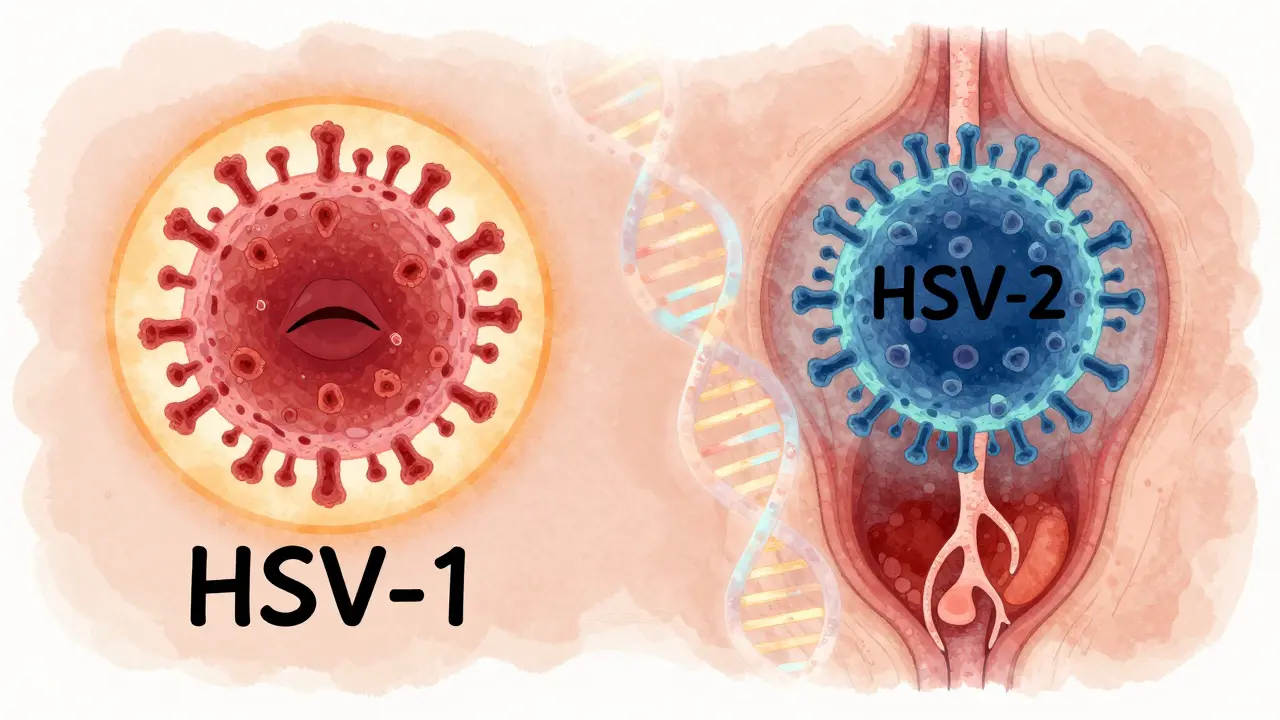
HSV-1 and HSV-2 are two strains of the same family of viruses. They look nearly identical under a microscope: both have a double-stranded DNA core wrapped in a protein shell and a fatty outer envelope. But their behavior? Totally different. HSV-1 used to be called the "oral herpes" virus because it mostly caused cold sores around the mouth. HSV-2 was labeled "genital herpes" because it stuck to the genitals. That’s changing.
Today, about 30-50% of new genital herpes cases in the U.S. and other high-income countries are caused by HSV-1 - usually from oral sex. Meanwhile, HSV-2 still causes 70-80% of genital outbreaks, but it’s also less likely to show up on the lips. The reason? Their preferred hiding spots in the body. HSV-1 settles into the trigeminal ganglion near your ear, ready to flare up on your face. HSV-2 hides in the sacral ganglion at the base of your spine, waiting to reactivate in the genital area.
They share about half their DNA, but that small difference changes everything. HSV-2 recurs more often - four to five times a year on average. HSV-1 genital infections? Most people have less than one recurrence per year. And when it comes to shedding - when the virus is active but you have no symptoms - HSV-2 is shed on 10-20% of days. HSV-1? Only 5-10%. That’s why suppressive therapy works better for HSV-2.
What Do the Symptoms Look Like?
First outbreaks are brutal. If you’ve never had herpes before, your body doesn’t know how to fight it. A primary HSV-1 infection in kids often looks like gingivostomatitis: fever over 38.5°C, swollen gums, mouth ulcers so painful you can’t eat or drink. Adults get it too - sometimes as a severe sore throat with blisters on the tongue and lips. You might feel dizzy, achy, or have bad breath. About 5-10% of these cases land people in the hospital.
Primary genital HSV-2 is even worse. Around 93% of people get painful ulcers. Most have trouble peeing because the sores sting. About 65% notice swollen lymph nodes in the groin. Fever hits 40% of cases. Vaginal or urethral discharge? Common. It’s not unusual to feel like you’ve got the flu - fatigue, muscle aches, chills - for days. These symptoms last 14-21 days without treatment.
Recurrent outbreaks are milder. The first sign? Tingling, burning, or itching in the same spot - usually just a few hours before blisters appear. Within a day or two, small fluid-filled bumps form. They turn into open sores, then crust over. Healing takes 5-10 days. You might not even notice if it’s just one or two tiny lesions. That’s why so many people don’t realize they have herpes until they get tested.
Not every outbreak looks the same. Some people get blisters. Others get just red patches. Some feel nothing at all. That’s why testing matters - especially if you’ve had unexplained sores or symptoms that come and go.
When Herpes Goes Beyond the Skin
Most people think herpes is just a skin issue. It’s not. HSV-1 is the leading cause of infectious blindness in the U.S. - herpes keratitis. It attacks the cornea. If untreated, it can scar the eye and lead to permanent vision loss. About 50,000 new cases happen every year. Treatment? Hourly antiviral eye drops for up to two weeks.
Then there’s encephalitis. Rare, but deadly. HSV-1 causes 95% of sporadic herpes encephalitis cases - inflammation of the brain, usually in the temporal lobe. Early symptoms: fever, confusion, seizures, strange behavior. Without treatment, half of patients die. Even with treatment, many are left with memory loss or personality changes.
Neonatal herpes is another terrifying risk. If a mother has an active genital outbreak during delivery, the baby can catch it. About 1 in 3,200 births in the U.S. results in neonatal herpes. HSV-2 causes 70% of these cases, but HSV-1 is deadlier - 30% mortality rate versus 20% for HSV-2. That’s why doctors recommend C-sections for women with active lesions at the time of labor. And why pregnant women with herpes are monitored closely.

How Is It Diagnosed?
Doctors don’t guess anymore. If you have a blister or sore, they swab it and send it for PCR testing. That’s the gold standard. It detects the virus’s DNA and gives results in 24-72 hours. It’s 95-98% accurate. Viral culture? Older tech. It only catches 70-80% of cases and takes longer.
What if you don’t have symptoms? Blood tests can tell you if you’ve been exposed. Type-specific tests like HerpeSelect or EUROIMMUN’s recomLine HSV IgG look for antibodies to HSV-1 or HSV-2. They’re 97-98% accurate after 16 weeks post-infection. But here’s the catch: if you test too soon, you’ll get a false negative. The body takes time to make antibodies.
And here’s the real problem: only 19% of people infected with HSV-2 in the U.S. even know it. Most never had a big outbreak. They think they’re fine. But they’re still shedding the virus - and still able to pass it on.
Antiviral Therapy: What Actually Works?
There are three main antivirals: acyclovir, valacyclovir, and famciclovir. They all work the same way - they block the virus from copying itself. But they’re not equal in how you take them.
For a first genital outbreak, the CDC recommends acyclovir 400mg three times a day for five days. That cuts healing time from 19 days to 10. Pain drops from 12 days to 8. Valacyclovir - a prodrug of acyclovir - is easier: 1g twice daily for the same five days. Famciclovir? 250mg three times daily. All three reduce transmission risk.
For recurrent outbreaks, you don’t need to take it for five days. Start within 24 hours of the first tingling, and take it for one to five days. If you catch it early, you might stop the outbreak before it even forms.
For people who get outbreaks more than six times a year, daily suppressive therapy is the best option. Valacyclovir 500mg once a day reduces HSV-2 transmission to partners by 48%. It also cuts outbreaks by 70-80%. That’s why doctors recommend it for couples where one partner is infected and the other isn’t.
For immunocompromised patients - those with HIV, cancer, or transplants - doses go up. IV acyclovir at 5mg/kg every 8 hours for mucocutaneous infections. For encephalitis? 10mg/kg. And if the virus becomes resistant? Foscarnet or the newer drug pritelivir. The FDA approved pritelivir in 2023 for acyclovir-resistant HSV. It cuts viral shedding by 87% in 48 hours.
For herpes eye infections, trifluridine eye drops are the go-to. One drop every two hours while awake. It’s harsh - stinging, blurred vision - but it works. Healing time drops from 21 days to 14.

Real People, Real Experiences
On Reddit, one user wrote: "First outbreak lasted 18 days. Fever hit 39.2°C. Twelve ulcers. Couldn’t pee without lidocaine." Then they started daily valacyclovir. "Now I get 2-3 day outbreaks with one or two tiny sores. It’s manageable."
Another said they got terrible nausea on acyclovir. Switched to famciclovir. No side effects. Control returned.
Drugs.com reviews show 82% of users say antivirals reduced outbreak duration. 65% say pain is much less. But side effects? Headache (22%), nausea (15%), and kidney issues in people with pre-existing conditions (8%).
But the biggest burden isn’t the physical symptoms. It’s the shame. A 2023 survey by the American Sexual Health Association found 74% of people with herpes feel anxious about stigma. 45% say it damaged relationships. 32% waited over six months to tell a partner.
What’s Next for Herpes Treatment?
There’s no cure yet. But things are changing. New drugs like pritelivir and amenamevir target the virus differently - not by blocking DNA copying, but by stopping it from unwinding. Early trials show they work faster than acyclovir.
Vaccines? Still in testing. GEN-003 and Simplirix showed promise in phase II trials, cutting viral shedding by 50%. But they’re not approved. The WHO is pushing for universal HSV-2 screening in pregnant women - which could prevent 1,200 neonatal cases a year in the U.S. alone.
Resistance is rising. In transplant patients, 15% of HSV strains now resist acyclovir. That’s why we need better diagnostics and smarter use of antivirals. Don’t take them unless you need them. Don’t skip doses. And don’t assume you’re safe just because you don’t have sores.
Herpes isn’t going away. But with the right knowledge and treatment, it doesn’t have to control your life.
Can you get herpes from kissing?
Yes. HSV-1 spreads easily through saliva, even when no sore is visible. Up to 50% of transmissions happen during asymptomatic shedding. Kissing someone with a cold sore is risky - but so is kissing someone who doesn’t know they carry the virus. Many people get HSV-1 as children from a family member’s kiss.
Is genital herpes always from sex?
No. While most genital HSV-2 cases come from sexual contact, HSV-1 genital infections are often from oral sex. You don’t need penetrative sex to catch it. Skin-to-skin contact with an infected area is enough. That’s why condoms don’t fully prevent transmission - the virus can be on areas not covered.
Do antivirals cure herpes?
No. Antivirals suppress the virus, reduce outbreaks, and lower transmission risk, but they don’t eliminate it from your nerves. Once infected, the virus stays in your body for life. That’s why daily suppressive therapy is about management, not cure.
Can you spread herpes without symptoms?
Yes. This is called asymptomatic shedding. With HSV-2, it happens on 10-20% of days. With HSV-1 genital infections, it’s 5-10%. That’s why people who never had an outbreak can still pass it on. Testing and suppressive therapy are the best ways to reduce this risk.
How effective is daily valacyclovir at preventing transmission?
For HSV-2, daily valacyclovir 500mg reduces transmission to uninfected partners by 48%, according to the Partners Transmission Study. For HSV-1 genital infections, the reduction is likely smaller because shedding is less frequent. Still, it’s the most effective tool we have - especially when combined with avoiding sex during outbreaks.
Are there natural remedies that work?
No credible evidence supports natural remedies like lysine, tea tree oil, or zinc for treating herpes outbreaks. Some may soothe skin temporarily, but none reduce viral shedding or prevent transmission. Relying on them instead of antivirals can lead to worse outbreaks and higher transmission risk.
Should I tell my partner I have herpes?
Yes. Ethically and legally, disclosure is required in most places if you know you’re infected. It’s not just about trust - it’s about shared health. Most partners are understanding, especially if you’re on suppressive therapy. Waiting too long increases the risk of unintentional transmission and deepens shame.
Can I still have kids if I have herpes?
Absolutely. Most women with herpes have healthy babies. The risk comes only if you have an active outbreak during delivery. Doctors monitor for symptoms near your due date. If you have sores or warning signs, they’ll do a C-section. If you’re on suppressive therapy, your risk of an outbreak at delivery drops to under 1%.
Final Thoughts
Herpes simplex virus is common, manageable, and rarely dangerous. It’s not a moral failing. It’s a virus. The real danger isn’t the sores - it’s the silence around it. The stigma keeps people from testing, from treating, from talking. Antivirals work. Transmission can be cut in half. Neonatal deaths can be prevented. Blindness can be avoided.
You don’t need to be ashamed. You just need to know the facts - and act on them.



Shelby Marcel, January 23, 2026
so i just found out my ex had herpes and i never knew... like wtf how do you not tell someone? i thought it was just cold sores lol
Gina Beard, January 24, 2026
It’s not a moral failing. It’s biology. But society turns it into a sin.
And the silence? That’s the real virus.
Patrick Gornik, January 26, 2026
Let’s be real - the medical-industrial complex profits from perpetual suppression. Acyclovir? A $200/month placebo with side effects. The real cure is epigenetic reprogramming, vagal toning, and gut microbiome recalibration. But nope - we’d rather pump pills into people than ask why their immune system surrendered in the first place. The virus isn’t the enemy. The paradigm is.
Luke Davidson, January 27, 2026
I had my first outbreak after a makeout session with someone who said they were 'clean'. Turned out they had HSV-1 and didn't know. Took me 3 weeks to heal. Started valacyclovir and now I get maybe one tiny thing a year. Honestly? It's not the end of the world. The shame is worse than the sores.
And yeah, condoms don't help much. Skin-to-skin is the real deal. But you can still have a full life. I'm married now. We talk about it. We're fine.
Kevin Waters, January 28, 2026
Just want to add - if you're on suppressive therapy and your partner is negative, you're doing everything right. Transmission risk drops to near zero with daily valacyclovir + no sex during outbreaks. Don't let fear silence you. Knowledge is power, and you're not alone.
Shanta Blank, January 30, 2026
I got herpes from my ex who swore he 'never had it'. He was lying. I cried for three days. Then I Googled neonatal herpes and almost threw my whole life away. Now I carry valacyclovir like a weapon. And I don't kiss anyone without asking. I don't trust anyone. Not even my mom.
They say 'it's manageable'. But what they don't say is: you'll never feel safe again.
blackbelt security, January 31, 2026
You don’t need to be ashamed. You need to be informed.
That’s it.
Jamie Hooper, February 2, 2026
mate i got herpes from a kiss at a party in 2019 and i still dont know if it was hsv-1 or 2. doc just said 'eh its fine'. now i get a tiny thing once a year if i get stressed. its not a big deal. why is everyone so dramatic?
Elizabeth Cannon, February 4, 2026
I'm a nurse. I've seen people cry because they think they're 'dirty'.
They're not. They're just human.
And antivirals? They're the closest thing we have to magic.
Use them. Talk about it. Protect your people.
You're not broken. You're just carrying a virus. And you're still worthy of love.
Tommy Sandri, February 5, 2026
The public health implications of asymptomatic shedding and inadequate screening are profound. While pharmacological suppression reduces transmission by nearly half, structural interventions - including universal prenatal screening and public education campaigns - remain underfunded and politically neglected. The stigma associated with HSV is not merely sociocultural; it is a systemic barrier to epidemiological control.