Every year, more than 1.3 million people in the U.S. end up in the emergency room because of medication mistakes. Many of these aren’t accidents - they’re the result of myths people believe are true. You’ve probably heard them: "Over-the-counter drugs are harmless," "If one pill helps, two will help more," or "I can stop my antibiotics once I feel better." These aren’t just harmless rumors. They’re dangerous. And they’re costing lives.
Myth: Over-the-Counter Medications Are Completely Safe
It’s easy to think OTC drugs are safe because you can buy them without a prescription. But that’s like saying a car is safe because you don’t need a license to drive it. Acetaminophen - the active ingredient in Tylenol and hundreds of other pain relievers - is the leading cause of acute liver failure in the U.S. Every year, about 56,000 emergency room visits, 26,000 hospitalizations, and 500 deaths are tied to acetaminophen overdose. The FDA lowered the recommended daily limit to 3,000 mg in 2011, but most people still think 4,000 mg is fine. That’s eight extra-strength tablets. One extra tablet a day, over time, can quietly damage your liver.
And here’s the tricky part: acetaminophen is in cold medicines, sleep aids, and prescription painkillers like Vicodin. You might take one for a headache, another for a cold, and a third for sleep - all without realizing you’ve hit the danger zone. The FDA now requires clearer warning labels on OTC products, but you still need to read every bottle.
Myth: Taking More Will Make It Work Better
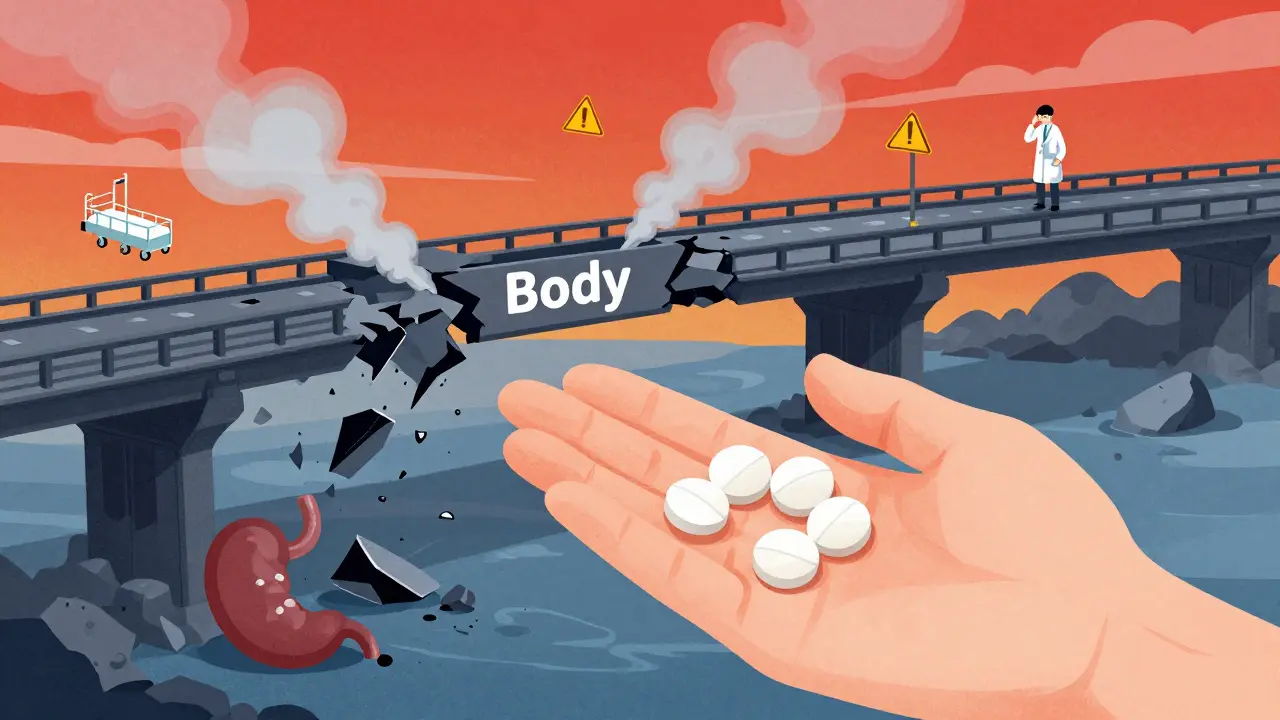
If one ibuprofen eases your headache, why not take two? Or three? It feels logical. But it’s not. The body doesn’t respond to higher doses like a volume knob - turn it up, and it gets louder. It responds like a bridge - push too hard, and it collapses.
Studies show that taking more than 1,200 mg of ibuprofen in 24 hours increases your risk of stomach bleeding by 4.5 times. That’s not a small risk. It’s a real, life-threatening one. And it’s not just ibuprofen. Naproxen, aspirin, and other NSAIDs carry the same danger. Your body doesn’t need more to work better - it just needs the right amount, at the right time.
Doctors don’t pick doses randomly. They’re based on decades of research, weight, kidney function, and other medications you’re taking. Taking more doesn’t mean faster relief - it means more side effects, more hospital visits, and more risk.
Myth: You Can Stop Antibiotics When You Feel Better
This is one of the most common and dangerous myths. You take antibiotics for a sinus infection. After three days, you feel fine. So you toss the rest. Why finish what you don’t need?
Because the bacteria you feel better from aren’t the only ones left. The strongest ones - the ones that survived the first few doses - are still there. And now, they’re stronger. That’s how antibiotic resistance starts. The CDC estimates that 35,000 people die each year in the U.S. from antibiotic-resistant infections. Many of those infections started because someone stopped their pills early.
Antibiotics don’t work like painkillers. They don’t just mask symptoms. They kill or stop the growth of bacteria. If you don’t finish the course, you’re not curing the infection - you’re breeding superbugs. The World Health Organization calls antibiotic resistance one of the top 10 global public health threats. Your decision to stop early affects not just you - it affects everyone.
Myth: Natural or Herbal Products Are Always Safe
"It’s natural, so it’s safe," people say. But poison ivy is natural. Deadly nightshade is natural. And so is St. John’s Wort - a popular herbal remedy for depression. Here’s the catch: St. John’s Wort can make birth control pills 15% to 33% less effective. That’s not a small risk. That’s an unintended pregnancy risk.
Another common herbal supplement, ginkgo biloba, is often taken for memory or circulation. But if you’re on blood thinners like warfarin, ginkgo can increase your bleeding risk by 50%. That means you could bruise easily, bleed longer from cuts, or even have a dangerous internal bleed.
Unlike prescription drugs, herbal products aren’t required to prove safety or effectiveness before they’re sold. The FDA only steps in after harm is done. So just because something is labeled "natural" doesn’t mean it’s safe to mix with your other meds. Always tell your pharmacist or doctor what supplements you’re taking - even if you think they’re harmless.
Myth: Mixing Alcohol with Medication Is Fine If You Don’t Drink Much
You have a glass of wine with dinner. You take your painkiller. You think it’s fine. But if that painkiller contains opioids - like hydrocodone or oxycodone - you’re playing Russian roulette with your breathing.
A 2020 study in Addiction Biology found that combining alcohol with opioids increases the risk of respiratory depression - when your breathing slows to dangerous levels - by 800%. That’s not a typo. Eight times more likely. And you don’t need to be drunk. Even one drink can be enough.
It’s not just opioids. Alcohol can make sedatives, sleep aids, antidepressants, and even some blood pressure meds work too well - leading to dizziness, falls, fainting, or worse. The University of Puget Sound’s prevention team calls this combination "extremely dangerous," and they’re right. There’s no safe level of alcohol when you’re on certain medications. If you’re unsure, ask your pharmacist. Don’t guess.

Myth: Generic Drugs Are Inferior to Brand Names
Some people believe generics are "cheap versions" - weaker, less effective, made with lower-quality ingredients. That’s not true. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand-name drug. They must be 80% to 125% bioequivalent - meaning your body absorbs them at the same rate and to the same extent.
Why are generics cheaper? Because the manufacturer doesn’t have to repeat expensive clinical trials. The safety and effectiveness were already proven by the brand-name version. The FDA inspects generic drug factories just as often as brand-name ones. In fact, many brand-name companies make their own generic versions.
Switching to a generic can save you hundreds a year - without sacrificing safety or results. If your doctor prescribes a brand-name drug, ask if a generic is available. If your pharmacist switches you to a generic, don’t panic. It’s not a downgrade. It’s a smart choice.
What You Can Do Right Now
Myths live because they’re repeated. They die when people ask questions. Here’s how to protect yourself and your loved ones:
- Do a brown bag review. Once a year, take all your medications - pills, patches, vitamins, supplements - to your doctor or pharmacist. They’ll spot duplicates, dangerous combinations, and expired drugs. Studies show this cuts medication errors by 63%.
- Use the 5 Rights. Before you take any pill, ask: Is it the right patient (me)? The right drug? The right dose? The right route (swallowed, applied, injected)? The right time? This simple check prevents most mistakes.
- Use the Teach-Back Method. After your pharmacist explains your new medication, say: "Can you explain this to me like I’m telling my spouse?" Then repeat it back in your own words. One study showed this boosted patient understanding from 42% to 89%.
- Sync your refills. If you take multiple prescriptions, ask your pharmacy if they offer medication synchronization. It means all your refills are due on the same day each month. One program increased adherence from 52% to 81% among older adults.
- Use trusted apps. Apps like Medisafe send reminders, track interactions, and alert you if you’re about to take a dangerous combo. Users report 37% fewer dosing errors.
Why This Matters
Medication errors aren’t just personal mistakes. They’re a system-wide crisis. Preventable adverse drug events cost the U.S. healthcare system $42 billion a year. That’s more than the annual budget of many states. And for every dollar spent on medication safety education, hospitals save $7 in avoided readmissions.
Pharmacists are your hidden safety net. They’re trained to catch mistakes before they happen. In 2023, U.S. community pharmacies addressed safety concerns on 50% of all 3.8 billion prescriptions dispensed - preventing an estimated 195 million medication-related problems. That’s not luck. That’s expertise.
The FDA, CDC, and pharmacists are working hard to fix this. But they can’t do it alone. You have to be part of the solution. Ask questions. Read labels. Don’t assume. Don’t guess. Your life - and the lives of people around you - depends on it.




anthony epps, December 16, 2025
So taking two Tylenol for a headache is basically gambling with your liver? Holy crap.
Souhardya Paul, December 17, 2025
This is exactly why I started doing brown bag reviews with my pharmacist every year. I found three duplicate meds and a bottle of expired muscle relaxers I’d totally forgotten about. Simple habit, huge safety win. Also, I always use Medisafe now - it saved me from mixing alcohol with my antidepressant last month. Seriously, people, just check your meds.
Kayleigh Campbell, December 18, 2025
"Natural" means nothing except "not regulated." Poison ivy is natural too. And yet somehow people think if it’s sold in a hippie store, it’s not gonna kill them. 🤦♀️
Andrew Sychev, December 19, 2025
People are dying because they think their grandma’s herbal tea is medicine. Meanwhile, the FDA is sitting on their hands waiting for someone to drop dead before they say "maybe don’t mix this with warfarin." We need real consequences, not just pamphlets.
Dan Padgett, December 20, 2025
Back home in Nigeria, we say "the body knows its own medicine." But here, I see people treating pills like candy - pop one, pop two, pop three. It’s not about willpower. It’s about how we’ve been taught to treat our bodies like machines you can just crank up. But we’re not cars. We’re living, breathing, fragile things. We need to listen, not just dose.
Hadi Santoso, December 21, 2025
just found out my "natural sleep aid" had st johns wort in it… and i was on birth control. like. wow. thanks for the surprise pregnancy risk, walmart. also, generic metformin saved me $200 a month. why do people still think brand name = better? it’s the same damn pill.
Randolph Rickman, December 21, 2025
Let me tell you - I used to think antibiotics were a cure-all. Got a cold? Pop some amoxicillin. Then I learned the hard way: I almost gave myself a C. diff infection because I stopped early. Now I finish every course, even if I feel fine. It’s not just about me - it’s about keeping antibiotics working for everyone. Don’t be the reason we lose them.
Josias Ariel Mahlangu, December 22, 2025
It’s not hard to read a label. If you can’t be responsible enough to check what’s in your medicine, maybe you shouldn’t be taking it. This isn’t rocket science. It’s basic human responsibility.
Arun ana, December 24, 2025
❤️❤️❤️ I’ve been telling my cousins in India this for years - "natural" doesn’t mean safe. My aunt took ashwagandha with her blood pressure meds and ended up in the hospital. Now she carries a list of all her meds to every doctor. Smart move. Everyone should do this.
Kim Hines, December 24, 2025
I used to think generics were fake. Then I switched to generic lisinopril and didn’t notice a difference. Same pill. Same results. Saved me $150/month. Why do we still believe the marketing?
Tiffany Machelski, December 26, 2025
did you know that some cold meds have acetaminophen in them? i didnt. and then i took tylenol and a cold pill and felt sick. i thought it was the flu. turns out it was my liver screaming. lesson learned.
SHAMSHEER SHAIKH, December 28, 2025
It is of paramount importance that the public be educated regarding the pharmacological implications of self-medication. The FDA, CDC, and professional pharmacists have issued numerous advisories - yet, the prevalence of medication-related errors persists due to a cultural ignorance of pharmacokinetics and bioequivalence principles. A systemic, community-based educational initiative is not merely advisable - it is imperative.
James Rayner, December 30, 2025
I used to think mixing wine with my pain meds was fine - I only had one glass. Then I passed out on the bathroom floor. My wife called 911. Turned out, the opioid in my prescription plus alcohol nearly stopped my breathing. I didn’t know. No one told me. Now I ask my pharmacist every time I get a new script. Don’t be like me. Ask. Always ask.