Splitting pills might seem like a simple way to save money or make swallowing easier, but it’s not as safe as it looks. Many people do it without thinking twice-especially older adults on multiple medications or those struggling with high drug costs. But a wrong cut can mean too much or too little medicine in your system. And that’s not just inconvenient-it can be dangerous.
Why People Split Pills
People split pills for three main reasons: cost, swallowing trouble, and lack of available dosages. A 10mg tablet often costs the same as a 5mg one. Splitting it gives you two doses for the price of one. For someone taking a daily blood pressure or antidepressant pill, that can mean saving $20 to $30 a month. According to GoodRx data from 2023, this practice saves Americans an average of $187 per year per medication. For seniors with arthritis or neurological conditions, swallowing large pills can be painful or even risky. Splitting them in half makes it easier. Some medications simply aren’t made in smaller doses. If your doctor prescribes 25mg of a drug that only comes in 50mg tablets, splitting becomes the only option. But here’s the catch: not all pills are meant to be split. And doing it wrong can lead to serious side effects.Which Pills Are Safe to Split?
The safest pills to split are scored, immediate-release tablets. A score line is that little groove down the middle of the pill. It’s not just for show-it’s a sign the manufacturer tested how the pill breaks and designed it to split evenly. Common safe medications include:- Citalopram (Celexa)
- Escitalopram (Lexapro)
- Fluvoxamine (Luvox)
- Sertraline (Zoloft)
- Amlodipine (Norvasc)
- Hydrochlorothiazide
- Atorvastatin (Lipitor)
- Metoprolol (Lopressor)
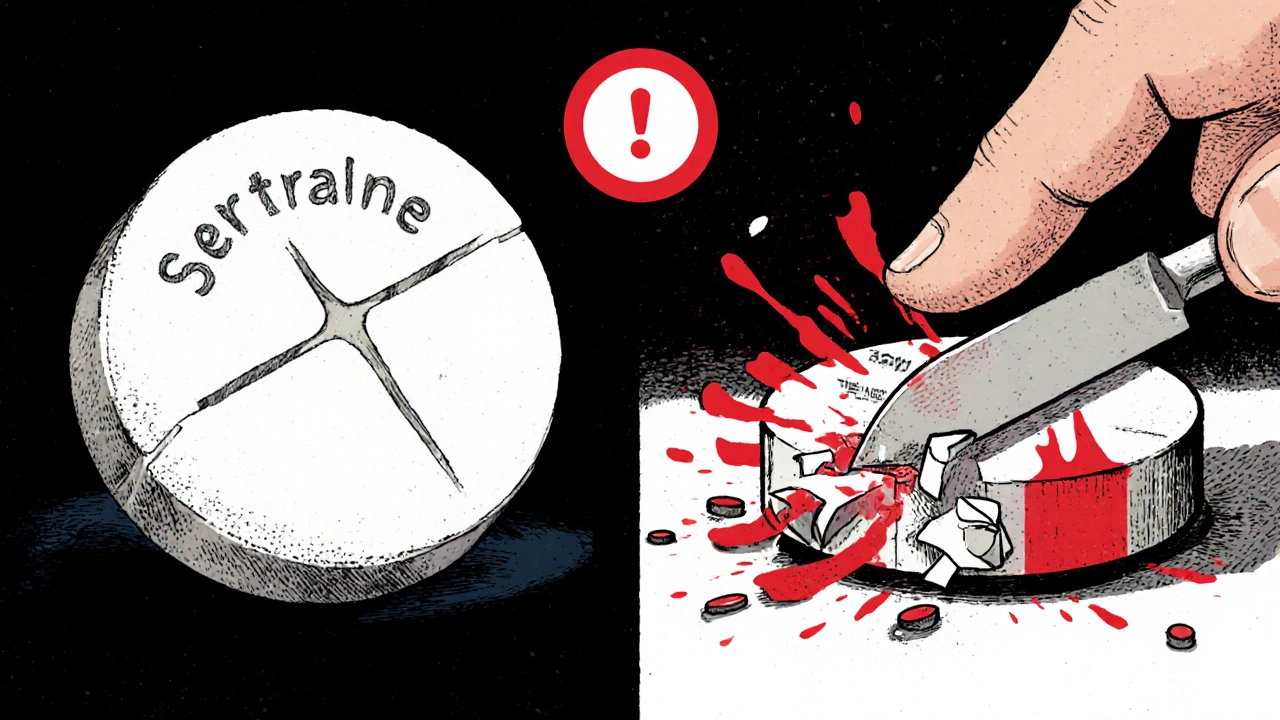
Which Pills Are NEVER Safe to Split?
Some pills are designed to release medicine slowly over hours. Splitting them destroys that system. You could end up taking the whole day’s dose all at once. That’s dangerous-even deadly. Never split:- Extended-release (ER), sustained-release (SR), or controlled-release (CR) tablets
- Enteric-coated tablets (they have a special coating to protect your stomach)
- Capsules with powders, gels, or pellets inside
- Hazardous drugs like chemotherapy agents
- Alendronate (Fosamax) - Splitting can cause severe throat or esophagus irritation
- OxyContin (oxycodone ER) - Splitting releases all the painkiller at once, risking overdose
- Dabigatran (Pradaxa) - Splitting affects blood-thinning levels dangerously
- Paroxetine (Paxil) - Classified as hazardous by NIOSH due to reproductive risks; even dust from splitting can be harmful
How to Split Pills Safely
If your doctor says it’s okay to split your pill, follow these steps:- Use a tablet cutter-not scissors, a knife, or your fingers. A $10 plastic cutter from the pharmacy is far more accurate than any improvised tool.
- Only split one pill at a time. Never split your whole month’s supply. Exposure to air and moisture can reduce potency by up to 35% in just three days.
- Store split halves in an airtight, opaque container. Light and humidity degrade medicine.
- Use the split half immediately. Don’t let it sit.
- Wash your hands before and after handling pills.
What Happens When You Split Wrong?
People often think, “It’s just half a pill-it can’t be that off.” But medicine isn’t like cutting a cookie. One study on hydrochlorothiazide (a water pill) found that when split with fingers, 12% of the halves were more than 15% off the target dose. That’s enough to cause dizziness, low blood pressure, or kidney issues. On Reddit, users reported dizziness and fainting after splitting amlodipine without a cutter. One man split his blood pressure pill with a knife and ended up in the ER with a heart rate of 120. The National Community Pharmacists Association surveyed 1,200 pharmacists in 2021. Sixty-three percent said they’d seen at least one patient incident linked to improper splitting in the past year. That’s not rare. It’s common.Cost vs. Risk: Is It Worth It?
Yes, splitting saves money. But is it worth the risk? For amlodipine, splitting a 10mg tablet saves about $28.50 per 90-day supply. That’s real savings. But if you split it wrong and end up with a fall or a trip to the hospital, the cost jumps to thousands. Manufacturers now make lower-dose versions of many drugs. A 5mg amlodipine tablet might cost 35-50% more than a 10mg tablet-but it’s 99.8% accurate. No guessing. No risk. For many people, the savings aren’t worth the danger. Especially for drugs with a narrow therapeutic index-where even a 10% dose change can cause toxicity or treatment failure.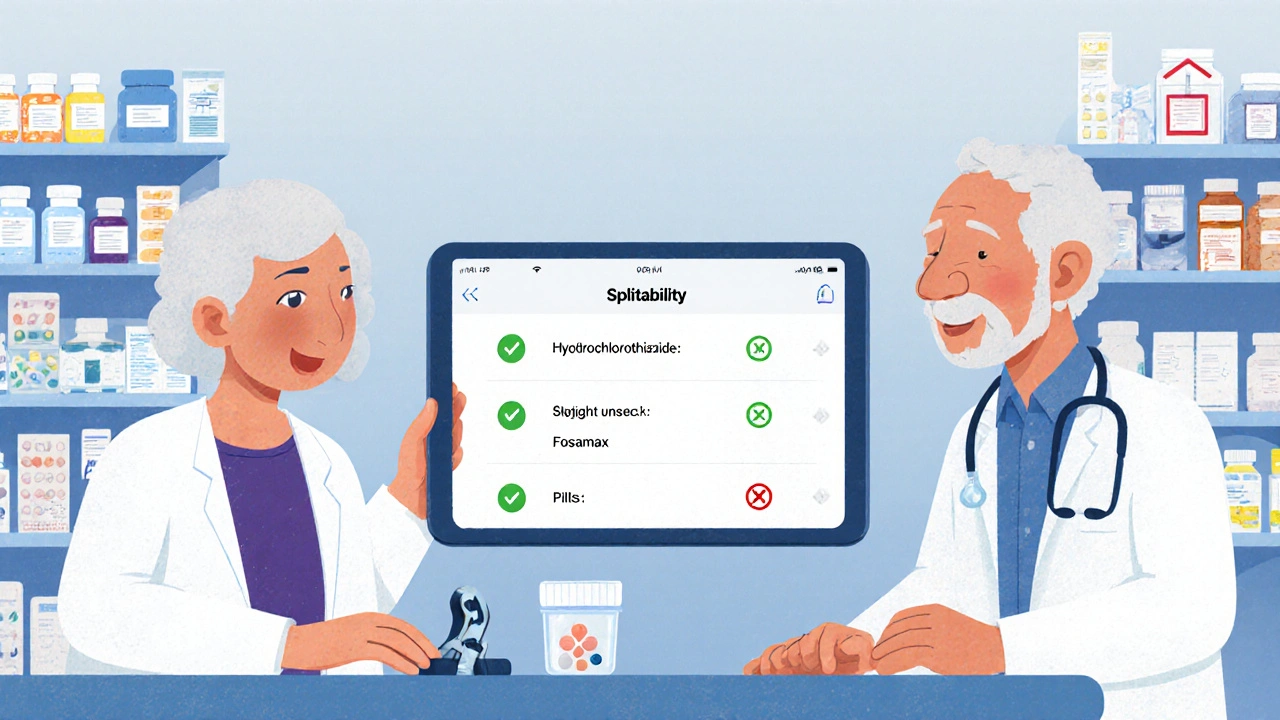
What Pharmacists Say
Most pharmacists don’t encourage splitting unless it’s clearly approved in the drug’s package insert. The National Community Pharmacists Association found that 78% of pharmacists routinely advise against splitting unless the label says it’s okay. Dr. Michael Cohen, president of the Institute for Safe Medication Practices, says the biggest mistake patients make is splitting their whole month’s supply at once. “You’re not just cutting a pill,” he says. “You’re exposing medicine to air, light, and moisture-and that changes how it works.” And it’s not just seniors. A 2022 Consumer Reports survey found that 41% of adults over 65 split pills without talking to a doctor or pharmacist. Those people had a 22% higher rate of medication-related problems than those who asked first.What’s Changing in 2025?
The FDA updated its guidelines in March 2023. Now, manufacturers must include splitability info in electronic drug labels. By December 2024, over 1,200 drugs will have this info clearly marked. Pharmacies are also rolling out apps that show you whether your pill can be split, how to do it, and what to watch for. Walgreens and CVS now offer these tools. One study showed they cut splitting errors by 29%. Still, 71% of hospital pharmacists remain concerned-especially for heart, seizure, and psychiatric meds. A tiny dose error there can be life-changing.Bottom Line: When to Split, When to Stop
You can split pills safely-but only under the right conditions:- Only split if your doctor or pharmacist says it’s okay.
- Only split scored, immediate-release tablets.
- Never split extended-release, enteric-coated, or capsule pills.
- Always use a tablet cutter-not scissors or knives.
- Split one pill at a time. Use it right away.
- Store split halves properly. Replace them every 72 hours.
Can I split my blood pressure pill in half?
You can split some blood pressure pills, like amlodipine or hydrochlorothiazide, if they have a score line and are immediate-release. But never split extended-release versions like Norvasc ER or Toprol XL. Always check with your pharmacist first. Splitting the wrong type can cause your blood pressure to drop too fast or spike unpredictably.
Is it safe to split pills with a knife or scissors?
No. Using a knife, scissors, or your fingers leads to uneven splits and inaccurate doses. Studies show dose variation jumps from under 10% with a tablet cutter to 25-72% with improvised tools. That’s dangerous for medications where even a small dose change can cause side effects or treatment failure.
Why do some pills crumble when I try to split them?
Some tablets are made with binders that don’t hold up well under pressure, especially if they’re old or exposed to moisture. This is common with low-cost generics. If your pill crumbles, don’t use it. Contact your pharmacist-they may have a better formulation or suggest an alternative.
Can I split my antidepressant pills?
Many antidepressants like sertraline, citalopram, and escitalopram are safe to split if they’re immediate-release and scored. But never split paroxetine (Paxil) or any extended-release version. Also, avoid splitting the entire month’s supply-do it one pill at a time to preserve potency.
What if I accidentally split a pill that shouldn’t be split?
If you split an extended-release, enteric-coated, or hazardous pill, stop taking it immediately. Call your pharmacist or doctor. You may need to switch to a different medication or dosage form. Don’t wait for symptoms-some risks, like overdose from OxyContin or esophageal damage from Fosamax, can develop quickly.
Are there alternatives to splitting pills?
Yes. Many drugs now come in lower-dose versions, liquid forms, or oral soluble films. These are more accurate and safer than splitting. Ask your doctor or pharmacist if a lower-dose tablet or alternative delivery method is available. Even if it costs a bit more, it’s often worth it for safety and consistency.



Chelsey Gonzales, November 23, 2025
lol i just used a knife for my amlodipine for years 😅 guess im lucky i didnt end up in the er
Charity Peters, November 25, 2025
my grandma splits hers with her nails. she says it’s easier than finding the cutter.
raja gopal, November 26, 2025
in india we often split pills because pharmacies dont always have small doses. but we always ask the pharmacist first. safety over savings any day.
Sarah Khan, November 27, 2025
the real issue here isnt whether you can split a pill-it’s that our healthcare system forces people into these risky compromises in the first place. if a 5mg tablet cost the same as a 10mg one, no one would be slicing tablets with butter knives at 7am while brushing their teeth. we’ve normalized medical austerity as a lifestyle choice, when it’s really a systemic failure.
the fact that 41% of seniors split meds without consulting anyone isn’t ignorance-it’s desperation. and the system rewards that desperation with pharmacy discounts while ignoring the downstream ER costs.
pharmacists are the unsung heroes here. they’re the ones catching the errors, the ones warning people, the ones quietly absorbing the emotional weight of someone saying ‘i just need it to last longer.’
the 2025 FDA labeling update? good. but it’s a bandage on a hemorrhage. what we need is price transparency, mandatory generic dosing options, and insurance coverage that doesn’t treat medication like a luxury item.
splitting pills is a symptom. the disease is affordability.
MaKayla Ryan, November 28, 2025
people are dumb. if you can’t afford your meds, get a better job. or move to a country that doesn’t bankrupt you for insulin. this country is falling apart because everyone thinks they deserve free stuff.
Faye Woesthuis, November 30, 2025
you’re not saving money. you’re gambling with your life. stop being reckless.
Crystal Markowski, December 2, 2025
if you’re splitting pills, please-please-use a cutter. they’re $8 at any pharmacy. i’ve seen too many patients with uneven doses, and it’s always avoidable. your health isn’t a budget spreadsheet.
Samantha Stonebraker, December 4, 2025
i used to split my sertraline like it was nothing-until i had a week of brain zaps and panic attacks that felt like my skull was cracking. turned out the tablet crumbled and i was getting maybe 30% of the dose. my pharmacist cried when i told her. not because she was upset, but because she’s seen this a hundred times. she gave me a free cutter and a new script for 25mg tabs. i cried too. not from sadness-from relief.
it’s not about being careful. it’s about being loved enough to have access to safe options. if your pharmacy doesn’t carry lower doses, ask them to order them. if your doctor says ‘it’s fine,’ ask them to check the FDA database. if you’re scared to ask-i’m here. you’re not alone.
Sondra Johnson, December 6, 2025
you ever try splitting a pill with a credit card on a kitchen counter? it’s like origami if the paper was made of regret and sodium chloride. i did it for six months on Lexapro-until my hands started shaking so bad i couldn’t hold the damn cutter. turned out i was getting 18mg one day, 2mg the next. my therapist asked if i’d been ‘feeling unstable.’ i said no. i just thought i was going crazy. turns out my brain was just starved of serotonin.
now i get the 10mg tabs. yeah, it costs $12 more a month. but i sleep. i laugh. i don’t stare at the ceiling wondering if i’m gonna faint. that’s worth more than a Starbucks.
and yes, i still keep the cutter in my purse. because i’m not the only one who needs it.
Kevin Mustelier, December 6, 2025
so… the FDA says by 2025 all pills will have splitability labels? that’s cute. but what about the 20 million people who still use expired pills from 2019? the ones with the sticky labels and the ‘use by 2021’ written in Sharpie? they’re not reading QR codes. they’re just hoping the pill doesn’t explode.
also, i split my metoprolol with a pizza cutter. it’s kinda satisfying. 🍕
Kelly Yanke Deltener, December 8, 2025
my mom split her Pradaxa because she thought it was ‘just a blood thinner.’ she had a stroke last year. the doctor said it was likely from inconsistent dosing. she’s in a nursing home now. i don’t care how much you save. if you split a pill you’re not supposed to, you’re not being smart-you’re being selfish. and you’re putting everyone who loves you through hell.
Kelly Library Nook, December 8, 2025
the statistical variance in dosing when using improvised tools is not merely a clinical concern-it is a pharmacokinetic catastrophe. the coefficient of variation for hand-split tablets exceeds 40%, which exceeds the therapeutic window for multiple cardiovascular and psychiatric agents. this constitutes a public health emergency of under-regulated self-administration. formal intervention, including pharmacist-led counseling and subsidized tablet cutters, is not merely advisable-it is ethically imperative.