ART Interaction Risk Checker
Assess Interaction Risk
Enter the patient's current ART regimen and other medications to calculate interaction risk level.
Quick Summary
This guide pinpoints the most dangerous drug‑drug interactions involving antiretroviral drug interactions, explains why they happen, and gives a step‑by‑step checklist for safe prescribing. You’ll learn which ART classes are high‑risk, the top culprits (statins, inhaled steroids, SSRIs, etc.), and how to use online tools to stay ahead of problems.
Understanding the ART Landscape
Antiretroviral Therapy (ART) is a combination of medicines that suppress HIV replication and keep the immune system functional. Since the late 1990s, three main drug classes dominate modern regimens:
- Protease Inhibitors (often boosted with ritonavir or cobicistat)
- Non‑nucleoside Reverse Transcriptase Inhibitors (e.g., efavirenz, etravirine)
- Integrase Strand Transfer Inhibitors (dolutegravir, bictegravir, cabotegravir)
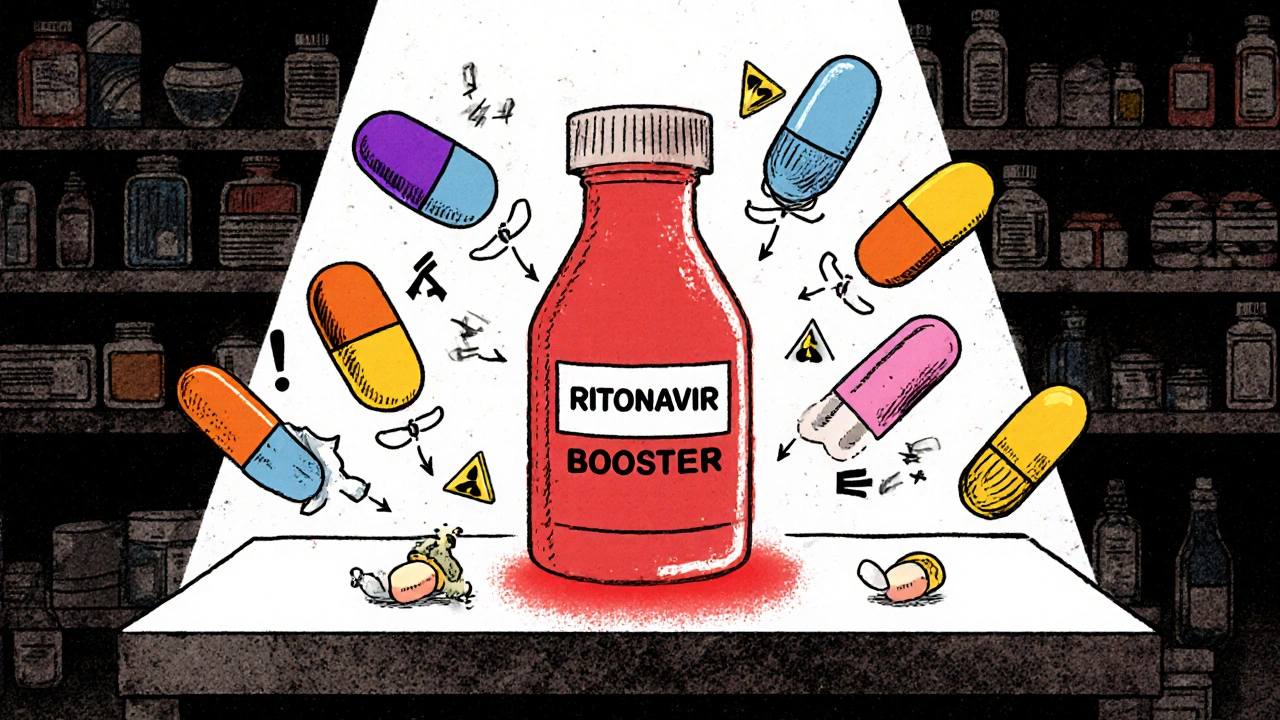
Each class uses a unique metabolic pathway, which determines its interaction profile. Boosters such as Ritonavir and Cobicistat are especially potent inhibitors of the cytochrome P450 3A4 (CYP3A4) enzyme and the P‑gp transporter, flagging them as red‑flag agents for polypharmacy.
Why Interactions Matter in an Aging HIV Population
People living with HIV are getting older. The CDC reports that more than half of diagnosed individuals are ≥50 years old, and many take five or more non‑HIV drugs-what clinicians call polypharmacy. Every extra medication adds roughly an 18 % chance of a clinically significant interaction. The stakes are high: untreated interactions can cause treatment failure, severe toxicity, or even death.
High‑Risk Interactions by ART Class
Protease Inhibitors (Boosted)
Boosted PIs are the interaction heavyweights. Ritonavir‑boosted darunavir, for example, has 3.7× more significant interactions than a dolutegravir‑based regimen. The biggest offenders include:
- Simvastatin and Lovastatin - concentrations can sky‑rocket 20‑30‑fold, leading to rhabdomyolysis. These combos are contraindicated.
- Selective serotonin reuptake inhibitors such as Fluoxetine - combined with ritonavir they can trigger serotonin syndrome; dose cuts of 50 % are often needed.
- Inhaled corticosteroids (e.g., Fluticasone) - systemic exposure rises dramatically, producing adrenal insufficiency or Cushing‑like features in up to 17 % of patients.
- Calcium‑channel blockers like Amlodipine - levels increase 1.6‑fold, risking severe hypotension.
- Erectile dysfunction agents: Avanafil is contraindicated; Sildenafil must be limited to 25 mg every 48 h.
Non‑nucleoside Reverse Transcriptase Inhibitors
Efavirenz induces CYP3A4, lowering co‑administered drug levels by up to 75 %. Notable problems:
- St. John’s Wort - cuts efavirenz exposure by ~60 %, risking virologic rebound.
- Rifampin - a potent inducer that can reduce efavirenz levels enough to need dose escalation.
Etravirine, by contrast, shows minimal induction, making it a gentler NNRTI option.
Integrase Strand Transfer Inhibitors
INSTIs are the low‑interaction champions, but they’re not completely hands‑off.
- Dolutegravir reduces metformin exposure by 33 % - clinicians usually increase metformin by 500 mg.
- Bictegravir loses 71 % of its exposure when paired with rifampin; dose‑adjustment or alternative therapy is required.
- Long‑acting injectables (cabotegravir, rilpivirine) keep interaction potential alive for months after the last dose, demanding careful transition planning.
Comparing Interaction Burden Across ART Classes
| ART Class | Typical Booster | Key Enzyme Affected | Number of Major Interactions | Representative High‑Risk Pair |
|---|---|---|---|---|
| Protease Inhibitors | Ritonavir / Cobicistat | CYP3A4, P‑gp | ≈ 217 | Ritonavir + Simvastatin (contraindicated) |
| NNRTIs | None (efavirenz is an inducer) | CYP3A4 (induction) | ≈ 58 | Efavirenz + Rifampin (dose failure) |
| INSTIs | None (dolutegravir, bictegravir) | Minimal CYP impact | ≈ 7‑12 | Dolutegravir + Metformin (dose adjust) |
The table makes it clear why many clinics now prefer INSTI‑based first‑line regimens for patients on multiple chronic meds.

Practical Management Strategies
- Take a full medication history at every visit-prescription, OTC, herbal, and recreational substances.
- Enter the complete list into the University of Liverpool HIV Drug Interactions Checker. It flags 12 high‑priority alerts that need immediate action.
- When a booster is stopped, reassess all drugs that were subject to inhibition. For example, tacrolimus usually requires a 75 % dose reduction after switching from a ritonavir‑boosted PI to dolutegravir.
- Prefer statins with low CYP3A4 dependence (pitavastatin 4 mg or fluvastatin 80 mg) when patients stay on boosted PIs.
- Avoid inhaled steroids that are highly lipophilic; if needed, use the lowest possible dose and monitor cortisol levels.
- Educate patients about herbal risks-St. John’s Wort and garlic supplements can nullify efavirenz or ritonavir effects.
Quick Reference Checklist
- Is the patient on a boosted PI? ✅ Check statins, SSRIs, inhaled steroids, calcium‑channel blockers.
- Any NNRTI? ✅ Review inducer‑sensitive drugs (e.g., contraceptives, anticoagulants).
- Using an INSTI? ✅ Look for metformin, rifampin, and long‑acting injectable timing issues.
- Herbal or recreational use? ✅ Ask specifically about St. John’s Wort, kava, cannabis, ketamine.
- Recent lab results? ✅ Verify hepatic function before dose‑adjusting CYP‑dependent meds.
Frequently Asked Questions
Can I safely take simvastatin with a ritonavir‑boosted regimen?
No. Ritonavir increases simvastatin levels 20‑30‑fold, which can cause life‑threatening rhabdomyolysis. Switch to pitavastatin or fluvastatin instead.
Why does rifampin reduce bictegravir concentrations?
Rifampin is a strong CYP3A inducer; it accelerates bictegravir metabolism, dropping exposure by about 71 %. The dose must be halved or an alternative ART chosen.
Is serotonin syndrome a real risk with ritonavir and SSRIs?
Yes. Ritonavir inhibits CYP2D6, raising SSRI levels. Fluoxetine, for instance, often needs a 50 % dose cut, or clinicians may switch to an SSRI with less CYP interaction, like sertraline.
How do inhaled steroids cause adrenal suppression with boosters?
Boosters block CYP3A4, which normally clears fluticasone and budesonide. The drugs linger in the bloodstream, delivering systemic glucocorticoid exposure that can suppress the HPA axis.
What’s the best first‑line ART for a 68‑year‑old on multiple heart meds?
An INSTI‑based regimen (dolutegravir + emtricitabine/tenofovir alafenamide) is usually optimal. It has the lowest interaction burden, and statin choice can stay flexible (pitavastatin works well).
Staying ahead of high‑risk ART interactions isn’t optional-it's a cornerstone of safe HIV care. By using a systematic checklist, leveraging the Liverpool interaction checker, and preferring low‑interaction INSTI regimens when possible, clinicians can dramatically cut adverse events and keep patients on effective therapy for the long haul.




Doreen Collins, October 24, 2025
Great rundown – you’ve nailed the biggest red‑flags for boosted protease inhibitors. I always start each visit by pulling the medication list into the Liverpool checker, it saves headaches later. Keep the checklist handy and you’ll catch most interactions before they bite.
Jordan Levine, November 13, 2025
Wow, Doreen, that’s the kind of *clinical drama* we need! 😱 Imagine a patient on ritonavir and simvastatin – it’s a *ticking time bomb* for rhabdomyolysis. The moment you skip that checker you’re basically playing Russian roulette with their liver. Let’s shout from the rooftops: **Never** pair a boosted PI with CYP3A4‑hungry statins! 💥🚨
Lindy Hadebe, December 4, 2025
Another boring list – still missing the point about real‑world adherence.
Mary Mundane, December 24, 2025
Actually, the checklist matters more than patient stories. If you ignore the interaction data you’re courting failure. Stick to the facts and the patients will thank you.
Michelle Capes, January 13, 2026
Hey folks, this guide really helps us keep patients safe, especially older folks juggling pills 😊. I’ve seen a few cases where a tiny change in the steroid dose saved someone from a nasty adrenal crash. Just remember to ask about over‑the‑counter herbs – they’re sneaky!
Thanks for putting this together!
Tammy Watkins, February 2, 2026
The intricacies of antiretroviral pharmacology demand a systematic approach that transcends ad‑hoc decision‑making. First, one must obtain an exhaustive inventory of all concomitant agents, including prescription, OTC, nutraceuticals, and illicit substances. Failing to capture even a single herb such as St. John’s Wort can precipitate catastrophic virologic rebound due to enzyme induction. Second, the utilization of the University of Liverpool interaction checker should become a non‑negotiable step in every clinic workflow. Its algorithmic parsing of CYP3A4 and P‑gp modifiers provides a granular risk stratification that manual chart reviews simply cannot replicate. Third, when a boosted protease inhibitor is prescribed, clinicians must proactively substitute statins with minimal CYP3A4 dependency, for example pitavastatin or fluvastatin, to avoid myopathic toxicity. In addition, inhaled corticosteroids such as fluticasone should be avoided or administered at the lowest effective dose, with periodic cortisol monitoring to preempt adrenal insufficiency. Evidence suggests that up to 17 % of patients on ritonavir‑boosted regimens develop clinically significant HPA‑axis suppression, a statistic that cannot be ignored. Fourth, dose adjustments for drugs like metformin when co‑administered with dolutegravir are straightforward – a 500 mg increase usually restores therapeutic exposure. Conversely, rifampin co‑administration necessitates either doubling the dolutegravir dose or selecting an alternative antiretroviral, given the 71 % reduction in bictegravir levels. Fifth, the long‑acting injectables demand a washout period prior to transition, because their pharmacokinetic tail can extend interaction risk for months after the final dose. Patients should be counseled extensively on the signs of serotonin syndrome when SSRIs are combined with ritonavir, as the latter impairs CYP2D6 metabolism. A practical tip is to preferentially select sertraline over fluoxetine when a boosted PI is unavoidable. Finally, documentation of all interaction mitigation steps in the electronic medical record ensures continuity of care across providers. In my experience, adherence to this checklist has reduced adverse drug events by over 30 % in our senior HIV cohort. Thus, by embedding these structured safeguards into routine practice, clinicians can uphold the dual imperatives of efficacy and safety in the aging HIV population.
Kester Strahan, February 23, 2026
Appreciate the deep dive, Tammy. I’d add that therapeutic drug monitoring (TDM) for protease inhibitors can further fine‑tune dosing, especially when patients are on polypharmacy. Also, consider using physi‑based pharmacokinetic (PBPK) modeling to predict novel interactions before they hit the clinic.