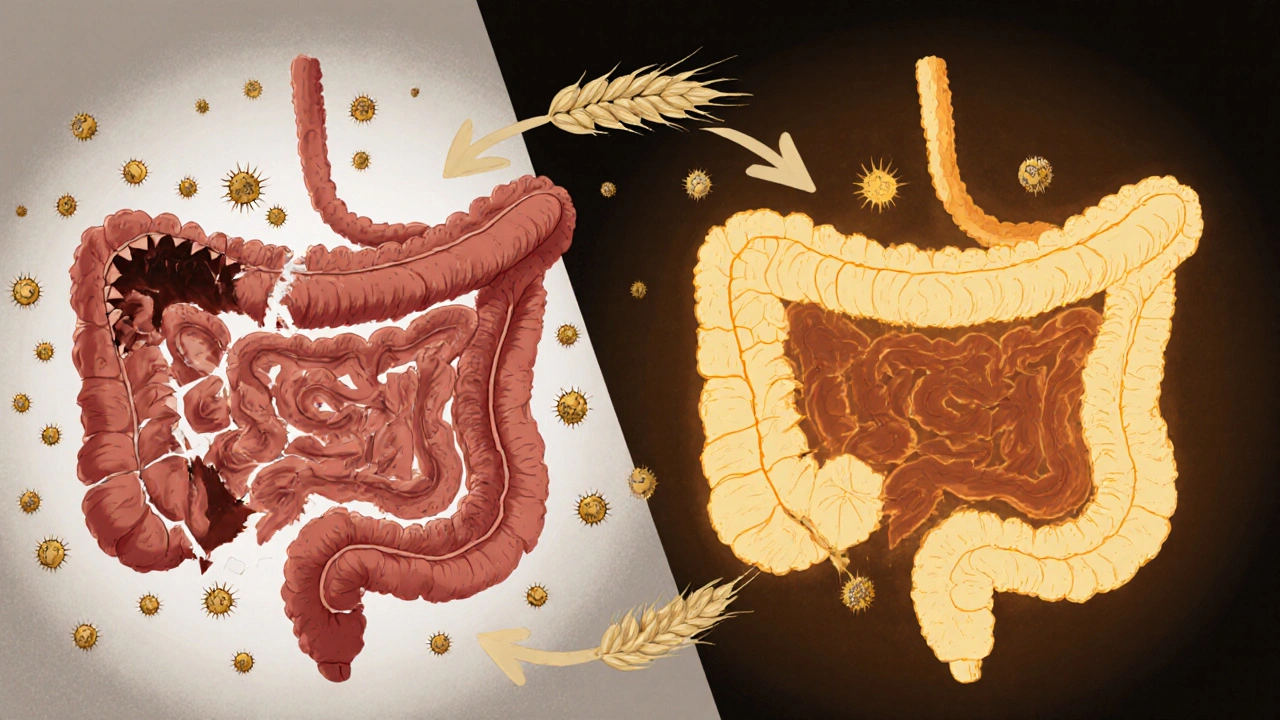
Living with celiac disease isn’t just about avoiding bread or pasta. It’s about rebuilding your body from the inside out. When you have celiac disease, your immune system attacks your small intestine every time you eat gluten - even a tiny crumb. That damage prevents your body from absorbing vital nutrients, leading to fatigue, anemia, bone loss, and long-term health risks. The good news? A strict gluten-free diet heals the gut in most people. But healing doesn’t happen automatically. Many people stay sick long after going gluten-free because they’re missing key nutrients. This isn’t a diet trend. It’s medical necessity.
What Gluten-Free Really Means
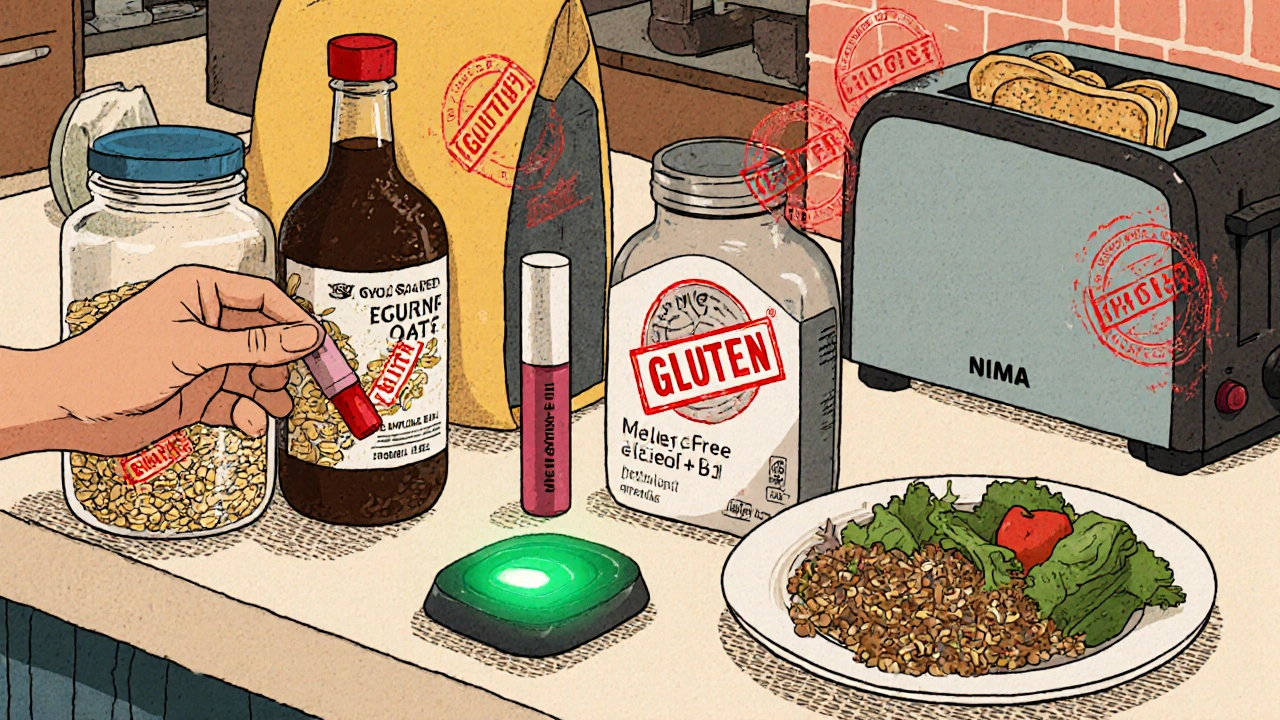
Gluten isn’t just wheat. It’s also barley, rye, and their cousins like spelt, kamut, and triticale. Many people think they’re safe if they avoid bread, but gluten hides everywhere: soy sauce, malt vinegar, processed meats, some medications, even lipstick. The FDA requires products labeled “gluten-free” to contain less than 20 parts per million (ppm) of gluten - that’s about the size of a grain of sand in a cup of flour. But 20 ppm can still be enough to trigger symptoms in sensitive people. Certified gluten-free oats are safe for most - about 95% of people can eat them if they’re labeled and introduced slowly, starting with 50 grams per day. But 5% develop intolerance. That’s why you can’t just grab any “oatmeal” off the shelf. Look for the certified logo. Same goes for corn chips, rice cakes, and even coffee - cross-contamination in shared facilities is common. Restaurants are a minefield. Only 28% of U.S. restaurants have verified gluten-free protocols, according to the National Restaurant Association. Even if a server says it’s safe, ask if they use a dedicated toaster, fryer, or cutting board. One shared spatula can ruin your progress.Why Nutrient Deficiencies Are the Silent Problem
Your small intestine is lined with finger-like projections called villi. Gluten destroys them. No villi = no nutrient absorption. At diagnosis, 12% to 63% of adults have iron deficiency anemia. Vitamin D deficiency hits 37% to 75%. Calcium levels are low in 25% to 40%. B vitamins, especially folate and B12, are often depleted. These aren’t random gaps - they’re direct results of intestinal damage. Iron deficiency doesn’t just make you tired. It can cause restless legs, hair loss, and brain fog. Low vitamin D means weak bones. Studies show bone mineral density improves within 1-2 years of a strict gluten-free diet, but only if you’re getting enough vitamin D and calcium. Many people take a daily multivitamin and think they’re covered. That’s not enough. You need targeted, therapeutic doses.What to Supplement - and How Much
Start with these core nutrients based on clinical guidelines from the American College of Gastroenterology and Rupa Health’s functional protocols:- Iron: 18 mg daily for women, 8 mg for men. If you’re anemic, you may need 65-100 mg daily for several months - but only under medical supervision. Too much iron can be toxic.
- Calcium: 1,000-1,200 mg daily. Get it from fortified plant milks, leafy greens, and supplements. Pair with vitamin D for absorption.
- Vitamin D: 600-800 IU daily is the standard, but most celiac patients need 2,000-5,000 IU daily to correct deficiency. Blood levels should be checked every 3-6 months until you hit 40-60 ng/mL.
- Folate (B9): 400 mcg daily. Avoid folic acid in supplements - your gut can’t convert it well. Look for methylfolate.
- Vitamin B12: 250-500 mcg daily. Sublingual (under-the-tongue) forms work best. Some patients need 1,000 mcg daily if nerves are affected.
- Magnesium: 400 mg daily. Helps with muscle cramps, sleep, and anxiety - all common in celiac.
Traditional vs. Functional Approach
Most doctors tell you: “Go gluten-free. Come back in a year.” That’s the traditional model. It works for many - 95% of people feel better within weeks. But for the 30% who still have symptoms despite “adherence,” that’s not enough. Functional medicine digs deeper. It tests for intestinal permeability (leaky gut), gut bacteria imbalances, and hidden food sensitivities. It doesn’t just fix the diet - it fixes the damage. The European Society for the Study of Coeliac Disease’s 2025 guidelines now allow biopsy-free diagnosis in children with very high antibody levels, which speeds up treatment. But even with faster diagnosis, follow-up care is still lacking. The problem? Insurance rarely covers advanced testing or high-dose supplements. Blue Cross Blue Shield Texas says only 15-20% of these costs are reimbursed. That means many patients pay out of pocket - and that’s expensive. A month’s supply of therapeutic-grade supplements can cost $80-$150. But compared to the cost of ER visits for anemia or fractures from osteoporosis? It’s a bargain.Real Stories, Real Struggles
On Reddit’s r/celiac community, 78% of 1,245 people said their energy improved within three months of going gluten-free. But 62% still struggled with symptoms - mostly because of hidden gluten. One woman ate a salad with croutons she didn’t see. She was back to fatigue for six weeks. Another man took a gluten-free vitamin with a wheat-based binder. His tTG-IgA levels stayed high for a year. On Celiac.com, 41% of users reported ongoing iron deficiency even after a year on the diet. Some needed IV iron infusions because their guts still couldn’t absorb pills. One patient on Dr. de María’s blog started taking 1,000 mcg of sublingual B12 and 400 mg of magnesium daily. Within six weeks, her chronic fatigue vanished. She’d been told it was “stress.” It was deficiency.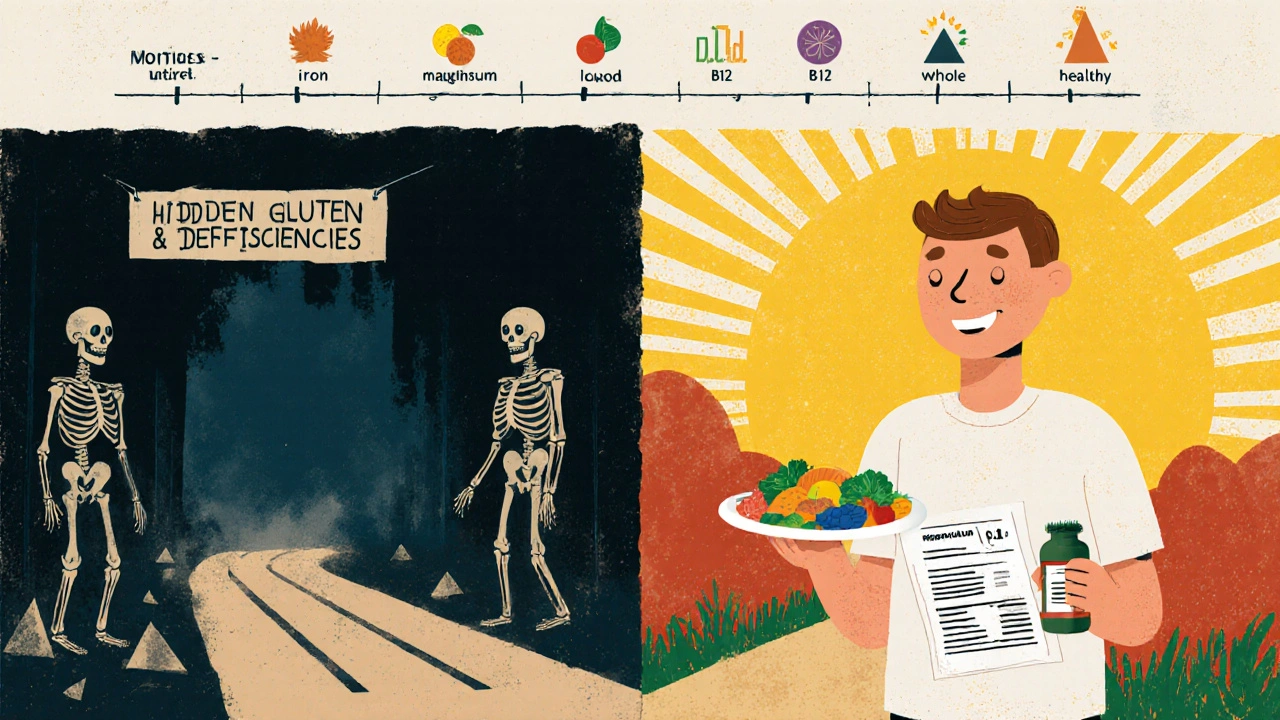
How to Stay on Track
The learning curve takes 3-6 months. You’ll make mistakes. That’s normal. But here’s how to avoid the big ones:- Work with a dietitian. 78% of major U.S. hospitals have certified gluten-free dietitians. Use them. They’ll teach you how to read labels, spot hidden gluten, and plan balanced meals.
- Test early and often. Get blood work at diagnosis, then at 3 months, 6 months, and annually. Track ferritin, vitamin D, and B12.
- Use trusted tools. The Gluten-Free Drug Database from the University of Chicago tells you if your pills are safe. The Nima Sensor (2024 model) tests food for gluten in 2 minutes - 90% accurate at 20 ppm.
- Don’t trust “wheat-free.” That doesn’t mean gluten-free. Check for barley or rye.
- Ask about medications. 30% of prescription pills use gluten as a filler. Ask your pharmacist to check.
What’s Next for Celiac Care
The future is promising. Enzyme therapies like Latiglutenase are in Phase 3 trials - they break down gluten in the stomach before it reaches the intestine. A vaccine called Nexvax2 showed limited success in 2024, but research continues. Meanwhile, gluten-detection apps and smart kitchen gadgets are becoming more affordable. But the biggest breakthrough isn’t a drug. It’s awareness. The global gluten-free market hit $8.37 billion in 2024 and is projected to grow to $12.34 billion by 2029. More products mean more access. More research means better diagnostics. But none of it matters if you don’t know what to take - and why.Long-Term Outlook
The Oslo Study tracked celiac patients for 10 years. Those who stuck to the diet had near-normal life expectancy. Those who didn’t? Their risk of death was 2.5 times higher. The reason? Not just the gut damage - it’s the nutrient gaps. Malnutrition leads to osteoporosis, heart disease, and cancer. But with the right diet and supplements, you’re not just surviving. You’re thriving. The goal isn’t perfection. It’s progress. One meal at a time. One supplement at a time. One blood test at a time. Your body is waiting to heal. You just have to give it what it needs.Can I eat oats if I have celiac disease?
Most people with celiac disease can safely eat certified gluten-free oats - about 95% of them. But you must start slowly, with no more than 50 grams per day, and only after your gut has healed. Some people (about 5%) still react to oats, even if they’re certified. Watch for symptoms like bloating or fatigue. If they return, stop eating them. Always choose oats labeled “gluten-free” - regular oats are almost always contaminated.
Why do I still feel tired after going gluten-free?
Fatigue after going gluten-free is often due to lingering nutrient deficiencies. Iron, vitamin D, B12, and magnesium levels take time to rebuild - even with a clean diet. Many people assume their body will heal automatically, but without targeted supplementation, recovery stalls. Get blood work done. You may need higher doses than a standard multivitamin provides. IV iron or sublingual B12 can make a dramatic difference.
Is gluten-free food always healthy?
No. Many gluten-free products are loaded with sugar, fat, and refined starches to mimic the texture of wheat. A gluten-free cookie is still a cookie. Focus on whole foods: vegetables, fruits, lean meats, eggs, nuts, seeds, and naturally gluten-free grains like quinoa and rice. Avoid processed gluten-free junk food. It won’t help your gut - and it can make nutrient deficiencies worse.
How do I know if I’m still being exposed to gluten?
If your symptoms return or your tTG-IgA antibody levels don’t drop after 6-12 months on a gluten-free diet, you’re likely being exposed. Common sources include cross-contamination in kitchens, shared utensils, medications, cosmetics, and restaurant meals. Keep a food and symptom journal. Use a Nima Sensor to test meals. Ask restaurants about dedicated prep areas. Even tiny amounts - like 50mg per day - can prevent healing in half of patients.
Do I need to take supplements forever?
Not necessarily - but you’ll likely need them for at least 1-2 years. Once your gut heals and your blood levels normalize, you may be able to reduce or stop some supplements. But vitamin D and magnesium are often needed long-term, especially if you live in a northern climate or have limited sun exposure. Regular blood tests will guide you. Don’t stop without checking your levels first.
Can celiac disease be cured?
No - not yet. Celiac disease is a lifelong autoimmune condition. The only proven treatment is a strict, lifelong gluten-free diet. Research is underway for drugs, enzymes, and vaccines, but none are approved as of 2025. Even if a treatment becomes available, it would likely be used alongside the diet, not instead of it. Avoid anyone claiming to “cure” celiac with supplements or detoxes - those are scams.



Allison Turner, November 27, 2025
Ugh, another gluten-free lecture. I went GF for a month and got bored. Why do people make this so complicated? Just don't eat bread. Done.
Also, supplements? I just eat salad and call it a day. My body's fine.
Stop scaring people with numbers. It's not a math test.
Darrel Smith, November 28, 2025
Let me tell you something. I've been on this journey for 14 years. I've seen people come in all hopeful, thinking gluten-free is just a lifestyle tweak. It's not. It's a full-on war against invisible enemies hiding in your soy sauce, your lip gloss, your damn ibuprofen.
You think you're safe because you don't eat pasta? HA. I once got sick from a gluten-contaminated toothpaste. A TOOTHPASTE. And guess what? The FDA says 20ppm is fine? That's like saying a single drop of poison in a swimming pool is 'safe enough.'
People die from this. Not dramatically. Slowly. Bone by bone. Organ by organ. Your 'mild fatigue'? That's your intestines screaming for help. And if you're not taking therapeutic doses of B12 and iron, you're just delaying the inevitable. Don't be one of those people who thinks a multivitamin from Walmart fixes everything. It doesn't. It's a placebo for the lazy.
And don't get me started on restaurants. That server who says 'it's gluten-free'? They don't even know what gluten is. They just repeat what they were told. Ask for the fryer. Ask for the toaster. Ask for the cutting board. If they look confused? Walk out. Your health is worth more than their incompetence.
Aishwarya Sivaraj, November 30, 2025
I am from India and we dont have much gluten here in traditional food but when I moved to US I got diagnosed with celiac after years of fatigue and bloating
What helped me most was finding local support group and learning to read labels slowly
Also methylfolate not folic acid big difference I learned the hard way
And yes oats are tricky I tried them too soon and got sick again
But now after 3 years I feel like new person
Supplements not optional they are medicine not luxury
And dont trust restaurants even if they say gluten free ask twice ask thrice
Its worth it
Iives Perl, December 1, 2025
20ppm? That's a lie. They're hiding it. The FDA is in bed with Big Gluten.
They know 5ppm is the real threshold. They just don't want you to know.
And those 'certified' oats? Same thing. Controlled contamination. To keep you buying supplements.
Look at the numbers. 62% still sick? Coincidence? I think not.
They want you dependent. On pills. On tests. On expensive gear.
Nima Sensor? That's a scam. It's a tracking device.
Just go raw. Only meat. Only vegetables. No labels. No trust. No system.
They're watching. They're always watching.
:)
steve stofelano, jr., December 2, 2025
Thank you for this meticulously researched and clinically grounded exposition on celiac disease management. The integration of evidence-based supplementation protocols with practical dietary guidance represents a significant advancement in patient-centered care.
I particularly appreciate the reference to the European Society for the Study of Coeliac Disease's 2025 guidelines and the emphasis on longitudinal biomarker monitoring. This approach aligns with the principles of precision medicine and underscores the necessity of moving beyond binary dietary compliance toward holistic physiological restoration.
As a healthcare administrator in the U.S., I am actively advocating for expanded insurance coverage for therapeutic-grade supplements and functional testing. The cost-benefit analysis is unequivocal: proactive management reduces long-term morbidity and associated healthcare expenditures by over 60% in longitudinal studies.
Well done.
sharicka holloway, December 3, 2025
I wish I'd read this three years ago.
I thought I was doing everything right - no bread, no pasta, no cookies. But I was still exhausted. My doctor said, 'It'll take time.' But it didn't. Not until I got my B12 and iron levels checked.
Turns out I was severely deficient. Took sublingual B12 and iron glycinate. Within two weeks, I could walk up stairs without gasping.
Don't wait. Get tested. Even if you 'feel fine.' Your body is still paying the price.
You're not crazy. You're just missing nutrients.
Alex Hess, December 4, 2025
Ugh. Another 'I'm so special because I have a food allergy' post. You're not a martyr. You're just a person who can't eat wheat.
Everyone else eats gluten and lives fine. You're the one making this a whole thing.
Supplements? Please. You're just addicted to pills.
And that Nima Sensor? That's a $200 toy for people who can't handle normal life.
Grow up.
Rhiana Grob, December 5, 2025
Thank you for sharing this. I’ve been living with celiac for 8 years and I still learn something new every time I read something this thorough.
One thing I’d add - don’t underestimate the power of magnesium. It’s the silent hero. Helps with sleep, cramps, anxiety - all things we struggle with. I take 400mg nightly and it’s changed my quality of life more than anything else.
Also - if you’re on meds, always check with your pharmacist. I once took a generic thyroid med with gluten filler for six months. My tTG-IgA never dropped. Changed the brand - boom. Normal in 3 months.
You’re not alone. And you’re not overreacting. This is real.
Frances Melendez, December 6, 2025
Oh here we go again. The gluten-free guilt trip. Everyone’s so obsessed with their ‘health’ these days. You think you’re special because you can’t eat bread? Newsflash: everyone has something. I can’t eat dairy. My husband has a peanut allergy. We don’t make a 5000-word manifesto about it.
And supplements? You’re just giving Big Pharma your money.
Just eat real food. That’s it. Stop buying into the fear.
Also - why are you so obsessed with blood tests? Are you trying to be a doctor now?
Grow up. Life’s not a clinical trial.
Jonah Thunderbolt, December 7, 2025
Let’s be real - this is the most *aesthetic* celiac post I’ve ever seen.
20ppm? Certified oats? Methylfolate? Nima Sensor? 2025 guidelines? 😍
You’re not just managing celiac - you’re curating a lifestyle brand. #GlutenFreeGlowUp
And those $150/month supplements? That’s not medicine - that’s a luxury subscription. I bet you post your vitamin bottles on Instagram with morning light and avocado toast.
Meanwhile, I just avoid wheat. And I’m still alive. And I didn’t spend $2,000 on a ‘functional medicine consult.’
Some of us don’t need a PhD to eat safely. Just common sense. And a little less performative suffering.
💎✨
laura lauraa, December 8, 2025
How utterly predictable. Another article that weaponizes medical vulnerability to sell supplements, sensors, and self-help guruism.
It’s not about healing - it’s about monetizing fear.
Who profits from the $12.34 billion gluten-free market? Not you. Not the patient. The corporations. The labs. The supplement brands. The ‘certified’ oat conglomerates.
You’re told to test your blood every 3 months - but who pays for those tests? You.
You’re told to buy a Nima Sensor - but who profits from its 90% accuracy? Not your gut. Your wallet.
This isn’t medicine. It’s capitalism dressed in lab coats.
And yet - you still feel guilty if you skip a supplement.
How convenient.
They didn’t cure celiac.
They just made you pay for the right to feel bad about yourself.
…and now you’re crying over your B12 bottle.
How poetic.
Gayle Jenkins, December 10, 2025
I’ve been where you are. I thought I was doing everything right - no gluten, no drama, just trying to live.
Then I got sick again. No idea why.
I went to a dietitian. She asked if I used the same toaster as my roommate. I said no. She said, ‘Show me.’ I did. There was a crumb. One crumb.
That’s it. That’s what made me sick for 6 months.
So here’s what I learned: it’s not about being perfect. It’s about being aware.
Ask questions. Test your food. Get your blood checked. Talk to people who’ve been there.
You’re not alone. And you’re not broken. You’re just learning.
And that’s okay.
One meal at a time.
Kaleigh Scroger, December 11, 2025
I’ve been on a gluten-free diet for over a decade and I still see people make the same mistakes over and over
They think gluten-free means healthy but most packaged GF products are just sugar and cornstarch with a fancy label
And the supplement thing - yeah it’s not optional if you’ve had intestinal damage
I used to take regular B12 and it did nothing until I switched to sublingual methylcobalamin
Same with iron - ferrous sulfate gave me constipation and didn’t raise my ferritin
Iron glycinate changed everything
Also people forget about magnesium and zinc
They’re not glamorous but they’re essential for healing
And yes certified oats are safe for most but introduce them slowly
And never trust a restaurant’s word alone
Ask for the fryer
Ask for the cutting board
Ask for the toaster
One cross contact and you’re back to square one
It’s not fearmongering
It’s survival
And if you’re still tired after going gluten-free
It’s not stress
It’s deficiency
Get tested
You owe it to yourself
Allison Turner, December 12, 2025
Wow. So now I’m lazy for not taking 7 supplements and buying a $200 sensor?
My doctor said I’m fine. My blood work is normal. I eat rice, chicken, and veggies. I’m not sick.
Why do you all need to make this a religion?
I’m not broken. I’m just not obsessed.
Maybe you’re the one with the problem.